HIV-Related Stigma and Discrimination in Jamaica: A Policy Review
Conducted in 2011 and 2013, this study in Jamaica explores the stigma, discrimination, and support experiences of individuals living with HIV. Findings highlight high levels of internalized stigma, experiences of exclusion and harassment, and challenges in disclosure. The study also assesses support systems and the influence of affected individuals on policy decisions.
Uploaded on Sep 19, 2024 | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
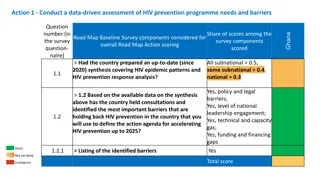
POLICY ISSUES RELATED TO HIV IN JAMAICA Stigma Index Study (2011) Review of the National HIV-related Discrimination Reporting and Redress System (2013) Situational Analysis of Patient Confidentiality within the Public Health Care Sector (2013) National Workplace Policy (2013) Originally presented at the first PHDP Training of People Living with HIV Peer Leaders Advocacy Workshop MODULE 17 Advocacy
Methodology Conducted August-September 2011 Across all four health regions Data collection using people living with HIV as interviewers and data entry clerks: Face-to-face survey Focus groups/case studies
Demographic Profile of Respondents Sample: N=509 Sex: 37% males and 62% females; 3 transgender (0.6%) Age: 8% <24 years; 9% aged 25-29; 34% aged 30-39; 29% aged 40-49; 19% 50+ Marital status: 47% single; 28% married; 20% in a relationship Education: 61% completed secondary school; 26% primary school Household size: 48% 1-3 persons; 35% 4-6 persons Few key populations identified: 87% identified with no key population group
Summary Stigma and Discrimination Experience One-third have experienced some form of discrimination in their communities High levels of internalised stigma Blame oneself, guilt, shame Have experienced social exclusion and self isolation Fears Gossip, verbal insults, physical harassment, physical assault Most fearful of neglect Experience psychological pressure and sexual rejection
Summary 2 Knowledge of support for people living with HIV Over one-third members of support organisations Only 9% involved in efforts to develop legislation, policies, or guidelines Close to half believe they cannot influence decisions in any area Disclosure Most are likely to disclose status to husband/wife/partner; adult family member; healthcare worker; social worker Least likely to disclose to friends/neighbours, religious leaders, community leaders, co-workers Reactions tend to be very supportive, with the exception of friends/neighbours
Confidentiality Medical records 52% not sure if medical record kept confidential 16% felt it was clear that medical record was not kept confidential Healthcare professionals 50% felt healthcare professionals never told others about status 39% not sure
Percentage of people living with HIV who report ability to influence decisions in any area (N=509) Area of influence N (%) Legal/rights affecting people living with HIVs Local projects intended to benefit people living with HIV National programmes/projects intended to benefit people living with HIV Local government policies affecting people living with HIV National government policies affecting people living with HIV International agreements/treaties Cannot influence decisions in any area 146 (31) 102 (21) 84 (18) 64 (13) 50 (10) 42 (08) 232 (46)
What support organisations should be doing to address stigma and discrimination (N=488) 4% Raise awareness/knowledge about AIDS Educate people living with HIV about living with HIV 20% 24% Advocate for rights of people living with HIV Provide support to people living with HIV 25% 25% Advocate for rights of most at-risk populations
REVIEW OF THE NATIONAL HIV-RELATED DISCRIMINATION REPORTING AND REDRESS SYSTEM (2013)
Context The extent and form of discrimination experienced by people living with HIV is not well documented. The extent and form of discrimination experienced by people generally, is not well documented. Discrimination is widespread and pervasive, but some discriminatory actions have become culturally acceptable and so they do not have the effect of causing the injured individual any offence.
The Review Funded by the USAID- and PEPFAR-funded Health Policy Project and supported by UNAIDS under the guidance of a steering committee led by the National HIV/STI Programme and JN+. Scope of Work: Conduct a gap analysis of the Redress System (NHDRRS) Make recommendations to address gaps and weaknesses Make recommendations to expand the system to include key populations The Process: Literature review (reports, evaluations, technical documents) Analysis of the legal and policy framework Meetings and consultations with key stakeholders SWOT analysis Stakeholder feedback
Recommendations (1) The NHDRRS should be integrated into the Organisational Structure of JN+: The NHDRRS will become the Client Complaints Arm of JN+. It would become part of the member services portfolio. A multi-sectoral Complaints Monitoring and Reporting Committee should be established as the accountability arm of the system. A cooperation arrangement should be entered into between JN+ and other HIV service organisation for resourcing the system. (Example the PSOJ/JEA/JBA/JCC Model). Day-to-day issues such as receiving complaints, setting appointments, and liaising with redress partners will be handled by a JN+ officer who will report to the committee. Volunteers, including attorneys who provide pro bono legal services, will also be part of the Monitoring and Reporting Committee.
What a Redress System Should Do Suggestions from focus group: Provide education and sensitization. Influence policies and legislation. Undertake or drive law reform and reforms in administrative practices. Court action. Provide legal assistance.
Proposed Structure of the NHDRRS Ministry of Labour and Social Security Police Civilian Oversight Authority Pharmacy Council of Jamaica Medical Council of Jamaica Complaints Monitoring and Reporting Committee JN+ Nursing Council of Jamaica Secretariat Office of the Public Defender Public Services Commission Ministry of Health and RHA Client Complaints Mechanism Mediation Other
Recommendations (2) Strengthen the technical capacity of JN+ The review recommends: An officer with legal or public policy/public administration skills. An officer with database management, statistical, and reporting skills. Data from focus group of people living with HIV (March 8, 2013): Counseling skills Legal skills (including knowledge of international human rights) Policy advocacy skills Interpersonal skills Knowledge of people living with HIV and gender equality issues
Recommendations (3) Use mobile digital technology NHDRRS needs an IMIT database Lobby for anti-discrimination legislation
Conclusions It is not sustainable to have a system dedicated exclusively to dealing with HIV-related discrimination. The discrimination complained of by people living with HIV can take place almost in relation to any person, based on almost any attribute: gender, race, age, abode. It is best to work through existing mechanisms which already have broad mandates. Public education and sensitisation are essential. Cooperation between JN+ and other service organisations is important given limited external resources and the broad reach of the NHDRRS.
SITUATION ANALYSIS OF PATIENT CONFIDENTIALITY WITHIN THE PUBLIC HEALTH CENTRE
Methodology A qualitative approach: Focus group discussions and interviews from key stakeholders Data collection from June 10 - July 5, 2013: Six focus group discussions Ten interviews
Findings 1. Definition of confidentiality 2. What constitutes a breach 3. Provider training issues 4. Health systems considerations (six sub- headings) 5. Framework for addressing breaches 6. Stigma and discrimination and its connection to confidentiality 7. Effects of breaches 8. Ethical dilemmas
Recommendations (1) 1. Leadership and Governance a. Prepare one policy document on patient confidentiality for the health services. b. Undertake a revision of the client complaint mechanism.
Recommendations (2) 2. Provider Training on Confidentiality Explore fully the role of professional bodies in training and enforcement of the issues surrounding patient confidentiality. Explore and integrate avenues of pre-service training on patient confidentiality. Revise the human resources approach to orientating and sensitising new staff on the issue surrounding patient confidentiality and develop strategies to reorient existing employees on preserving and maintaining patient confidentiality. a. b. c.
Recommendations (3) 3. Quality Assurance a. Develop and institute quality indicators specific to confidentiality per key groups with reporting schedules outlined for delivery in high-level leadership and governance forums. b. Ensure adherence to existing policy and procedures aimed at facilitating patient confidentiality.
Recommendations (4) 4. Infrastructure Continued infrastructural renovations to health facilities to facilitate improved privacy particular in A&E (emergency) and pharmacy departments. a. 5. Regulatory Body for Advocacy and Monitoring Explore the establishment of an independent regulatory body to advocate, monitor, highlight, and report confidentiality concerns. Bringing public attention both local (civil society) and international to the matter. a.
Recommendations (5) 6. Research Explore further the issues of confidentiality in the health sector with service users and employ the use of observation of services. Management of Health Information System a. 7. Convene a panel of experts to discuss the intricacies of how the Ministry of Health will address the paper-based storage of health records. a. Either enforce the regulations and procedures regarding the transfer of health records or widen the categories of person who can transfer health records and stipulate and enforce the safeguarding of the information being transferred. b.
Recommendations (6) 8. Integrated Health Service Delivery a. Clarify the concept and breath of the treatment team. b. Examine the issues involved in providing care to providers in a confidential manner and explore strategies to safeguard their information. c. Continue the process of integrating clinics and limit the ability to deduce and conclude information from existing systems and structures.
Recommendations (7) 9. Human Resources in Health a. Conduct a review of the documented roles and functions and the actual day-to-day activities of the following categories of staff: security guards, porters, and district constables. b. Establish guidelines that stipulate the locations within health facilities where student employees can be placed. Areas that limit access to health information are recommended.
Recommendations (8) 10. Health Information System a. Explore the feasibility of incorporating an electronic-based system with the necessary security features to limit access to patient information especially for larger health centres. b. Conduct a patient flow analysis that examines the movement of patient health records and other patient information within health facilities and determine the number of and categories of persons (health and non-health) who handle patient information and their suitability to access such records.
A Rights Based Approach to HIV and AIDS in the Workplace HIV Unit, Occupational Safety and Health Department Ministry of Labour and Social Security
Background HIV, which leads to AIDS, impacts the workforce nationally, regionally, and internationally. The most affected persons are those aged 15-49 years. Locally this age range accounts for more than 60% of reported HIV cases.
HIV/AIDS: A Workplace Issue In 2007, AIDS was one of the leading causes of death in the Caribbean. Globally, and within the Caribbean region, the highest number of AIDS cases occur in the 15-49 age group.
The Governments Response to HIV Led by the Ministry of Labour and Social Security In 2007 the National Workplace Policy on HIV and AIDS was developed. In 2010 the policy was approved as Green Paper by both houses of Parliament. In 2013 the policy was approved as White Paper by both houses of Parliament.
Key Principles: International Labour Organisation Code
Why Focus on Workers? When adults are well enough to work household well-being improves and health costs are reduced. Companies incur fewer costs from absenteeism, retraining, and recruitment. Source: Joint United Nations Programme on HIV/AIDS (UNAIDS). 2012. Together We Will End AIDS. Geneva: UNAIDS.
What can we do in the workplace? Reduce the impact of the epidemic on business. Reduce personal risk to infection. Reduce stigma and discrimination against workers living with and affected by HIV and AIDS and ensure their human rights in the workplace. Contribute to the goal of universal access to prevention, treatment, care, and support.