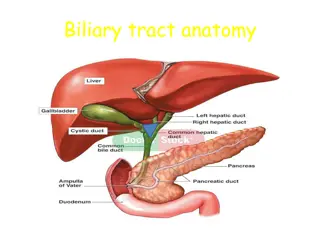
Gall Bladder and Bile Duct
The gall bladder and bile ducts play crucial roles in the storage and transportation of bile in the body. They have specific anatomical divisions and functions, including bile secretion, concentration, and storage. Understanding their structure and function is essential for grasping their physiological significance in digestion and overall health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
ANATOMY AND PHYSIOLOGY The gall bladder is pear shaped ,7.5 12 cm long. normal capacity 50 ml but it capable to distension in certain pathological conditions . Anatomical division are funds ,body, neck that terminate in narrow infindibulum cystic duct ; 3cm in length but variable ,lumen 1-3 mm diameter ,mucosa of duct arrange in spiral form producing valve of heister . Common hepatic duct; usually less than 2.5 cm long its form by union of rt and lf hepatic ducts its join with cystic duct to form common bile duct in 80 % supra duodenum
Common bile duct ; about 7.5 cm in long its divided in 4 parts 1- supra duodenum part about 2.5 cm run in the free margin of lesser omintum 2- retro duodenum part 3- infra duodenum part 4- intra duodenum part which surrounded by sphincter of oddi and open in summit ampulla of vater
Blood supply Cystic artery which branch from rt hepatic artery ,occasionally accessory cystic artery branch from gastro duodenum artery .usually cystic artery run behind common hepatic duct ,only 15% pass in front of this duct , Caterpillar turn anomalies : hepatic artery take tortuous form in front of the origin of cystic duct ,or the hepatic artery tortuous and cystic artery short.
Lymphatic drainage Of gall bladder to the cystic lymph node of lund (sentinel lymph node what means??)which located at the junction of cystic duct with common hepatic duct ,efferent vessels go to the liver hilum and to the celiac l.n Physiology Liver execrate bile at rate 40 ml / h ,bile compose from 97% water, 1-2% bile salt and 1% pigments, cholesterol and fatty acid. secretion of bile under control of cholecystokinin which release from duodenum mucosa.
Function of gall bladder 1- as a reservoir of bile 2- concentration of bile by active absorption of water, sodium chloride ,bicarbonate 3- secretion of mucus about 20ml /day
Bile composition and function Bile is a combination of cholesterol, phospholipids (mainly lecithin),bile salt, water, and conjugated bilirubin (break down product of HG),the bile salt reabsorbed in the distal small bowel ,pass back via portal venous system to the liver from where they are once again secreted in the bile ,this called entero hepatic circulation about 10 time a day, so in obstructive jaundice what will happened ??(fat and fat soluble vitamin A,D,E &K)
Investigation of biliary tract PLAIN X RAY---10% radio opaque of gall stones , calcification of gall bladder ( porcelain gall bladder) it premalignant condition and need cholecystectomy , gas in wall of gall bladder (emphysematous cholecystitis) ,gas in biliary tree a after endoscopic sphenectrotomy ORAL CHOLECYSTOGRAPHY -- Mainly used to assess the function of g.b and to show diverticuli and polyps , This test most of hospital not used because of inaccuracy . INTRAVENOUS CHOLENGIOGRAPHY Also not widely used because of contrast agent can cause allergic reaction Ultrasonograhpic Non invasive and now is the standard initial technique for the investigation of pt suspected to have g. stone. By this test can visualize g.b ,cbd, diameter pancreas ,
Radioisotope scaning Mainly used to assess biliary -enteric anastomosies ,we used 99Tc Ct; Ct; This test not useful in investigation of biliary tract ,only useful to detect gb gb and bile ducts tumor. Magnatic resonance cholengiopancreatography (mrcp) It s the stander technique in investigation of biliary tree ,contrast is not necessary. Endoscopic retrograde cholengiopancreatography ( ( ercp Done through ampulla of vater its diagnostic and therapeutic test This test may cause acute cholingitis. ercp)
Percutanous transhepatic cholengiography ptc Under fluoroscopic control a needle 15 cm long and 0.7 mm in diameter is passed to the liver through the 8 intercostal space in the mid axillary line . Contraindication of this procedure bleeding tendency and prophylactic antibiotic should be given prior to the procedure. Congenital anomalies For g. g.b b *absence of g.b *duplication of g. because of long mesentery which liable to torsion *phrygian cap 2-6% For cystic duct *absence of cystic duct, gb open directly to the bile duct *long cystic duct 10% of cases in which cystic duct open to the cbd near the ampulla f vater Cbd Cbd * cystic dilatation of the main bile ducts (choledocal cyst) Congenital obliteration of the ducts (biliary atrasia ) For b.v anomalies----* common about 25 % as cater anomalies ptc g.b b * floating g.b
Extrahepatic biliary atrasia Its occur in 1/14000 live births m/f ratio equal ,in this condition extra hepatic biliary duct progressively destroyed by inflammatory process ,intra hepatic billiary changes also occur and result in biliary cirrhosis and portal hypertension. Inflammatory destruction of biliary ducts classified to three main parts Type 1 ; atrasia restricted to cbd Type 2 ; atrasia of common hepatic duct Type 3 atrasia of rt and lf hepatic duct Main c. c.f f is progressive jaundice which start from 1st wk of life and signs and symptoms of obstructive jaundice
d. d.d d any form of jaundice in neonate such as 1- &1 antitrypsin deficiency 2- cholestesis associated with i.v feeding 3- choledocal cyst 4- inspissated bile syndrome 5- neonatal hepatitis Treatment Direct roux-en-y anastamosis in type 1 Type 2 &3 treat by kasia procedure (excision all biliary tract up to the liver capsule and roux- en-y done), bad prognosis
Choledocal cyst Is due to specific weakness in a part of or the whole of the wall of the common bile duct, Its associated with high biliary amylase in 80 % of cases because biliary pancreatic junction usually involved and may cause repeated pancreatitis Diagnosed by us and confirm diagnosis by mri .this condition is premalignant Treat by roux-en-y loop of jejunum
Types of choledochal cyst; TypeI ;difuse cystic and may extend into pancrease TypeII;diverticulum of CBD Type III; diverticulum within pancreas Type IV; extension into the liver Type V; cystic dilatation of only intra hepatic duct Treat by roux-en-y loop of jejunum
Gall stones Are the most common biliary pathology there are 3 types of stones 1- cholestrole stones 20 % its either solitary or as a2 stones or may be multiple in which associated with strawberry g.b 2- bile bigment 5% small ,black, irregular, multiple, and fragile 3- mixed stones 75% multiple, faceted, Other classification ; cholesterol, black pigment, brown pigment Causative factor in g.stones formation
a- bile stasis b- infection c- metabolic ; solubility of cholesterol depend on the concentration of phospholipids and bile acid in bile and on the type of phospholipids and bile acid ,so any change in these 2 factors leads to precipitate insoluble cholesterol pigments stones contain less than 30% cholesterol ,they are 2 types *black and brown black largely compose of insoluble bilirobin pigments usually occur in haemolysis . brown stones rarly seen in the gall blaader they form in bile ducts and related to bile stasis and infection
the effect and complication of gall stones in the g. g.b b;;; * silent stones * acute cholecystitis * chronic cholecystitis *gangrene * perforation** empyemia * mucocele * carcinoma in the bile ducts;;;;* obstructive jaundice * cholengitis * acute pancreatitis in the intestine --*acute intestinal obstruction ( gall stone illus)
acute calculus cholecystitis this due to impaction of gall stone to the out let of g.b ( cystic duct) so pt complaing from pain in rt hypochondrium area .colicky in nature because of obstruction , fever, nausea , vomiting, o/ o/e e tender upper abdomen often palpable mass may feel because of distended g.b and omentum surround it . if obstruction not relived there may be empyemia or even perforation of g.b will occur. d. d.d d -- 1- acute appendicitis 2- perforated d.u 3- acute pancreatitis 4- rt side basal pneumonia 5- coronary thrombosis.
Treatment Conservative treatment fallow by cholecystactomy 90% of patients will response to treatment which include *nasogastric aspiration and i.v fluid * analgesia * antibiotics brood spectrum a.b e.g cefazolin *after subsiding inflammation then cholecystectomy may be performed later on . Conservative management must be stop when the temp. increase ,pain ,,and mass increase in this condition percutanous cholecustostomy done under u/s control will resolve symptoms and later cholecystectomy . Some surgeons advocate urgent operation within 48 hours of acute attack ,good results we obtain if a good and experience surgeon .conversion rate of laparoscopic cholecystactomy 5 times in acute inflammation.
Mucocele of gall bladder This condition occur when there is obstruction of cystic duct by stone or tumor in which g,b filled with mucous that secreted from g.b mucous epithelium contain of g.b remain sterile .gb may become palpable. Empyema of of g, g,b b g.b filled with pus .it may be due to a sequel of acute cholecystitis or mucocele become infected ,treatment is drainage and later cholecystectomy. Acalculous cholecystitis This condition occur in patients recovery from major surgery ,trauma, and burn , There is high rate of miss diagnosis and carry high rate of mortality rate.
Cholecystactomy Preparation for surgery 1- assess fitness of pt to general anesthesia which include investigation to assess ,c.v.s. respiratory system,, liver function test blood coagulation, prophylactic antibiotic ,heparin sc or anti embolus stoking Sign a consent after explain to the pt why, when ,where and who to do the operation and intra and post operative complication that may occur. Open procedure Laparoscopic procedure Some golden role in case of difficulty 1- when anatomy of calot triangle is un clear blind dissection should stop 2- bleeding near the triangle should control by pressure not by blind clamp 3-when there is a doubt about the anatomy funds first cholecystactomy dissection of g.b 4- if suspected mirizzi syndrome (cystic duct adherent to cbd) must open infundibulum and remove stone then over sewn the infundibuluim.
Indication for choledochotomy 1- palpable stone in cbd 2- dialated cbd abnormal liver function test particularly alkalin phosphatase 4- jaundice or history of jaundice or cholengitis Post cholecystactomy syndrome In 15 % of pt cholecystactomy fail to relieve the symptoms this due either to miss diagnosis or due to presence of stone in cbd ,stone in cystic duct stump or operative damage to biliary tree so this best performed by mrcp 3- mrcp or or ercp ercp
Management of bile duct obstruction Pt complained from symptoms immediately after cholecystectomy or delayed need urgent investigation to diagnosed the cause .firstly we do urgent u/ sub hepatic collection or any dilatation of cbd , then immediate ercp of cbd . if stone present can removed endoscopically ,if collection of bile drain can pus percutaneously . and if possible pass stent in the bile duct. u/s s to see if ercp to see patency
Stones in the bile duct Duct stone may occur many years after acholecystectomy or be related to development of new pathology as infection or stasis of bile Symptoms May be asymptomatic or give charcot's triad(pain, fever, jaundice) Managements First must diagnosed the cause of jaundice either stone in cbd or due to hepatitis or due to seclorosing cholengitis , u/s ,liver function test, liver biopsy, if duct not dilated . pt is so ill and pus may be present in biliary tree, so drainage is important with good rehydration ,broad spectrum antibiotic and correct clotting factor . Drainge through ercp papilotomy and sphentrotmy ,if stone can removed through dromia basket. Or placement of stent if stone cannot removed . If technique failed pc cholengioscopy wes done
Choledochotomy This indicate when pt have obstructive jaundice due to stone in cbd and minimally invasive technique is un available so open choledactomy is indicated. after removal of stone t tube was put to drain cbd for 2 wks . or till bile become clear and general condition of pt become better t.tube cholengiography done if stone still present we leave the tube for 6 wks to create a mature fistula through which can remove stone.
Stricture of Stricture of cbd Causes of benign stricture Congenital biliary atrasia Bile duct injury --- cholecystectomy , choledochotomy, gastractomy ,hepatic resection, transplantation Inflammatory -- stones, cholengitis, parasitic, pancreatitis seclorosing cholengitis, radiotherapy Trauma Idiopathic Radiological investigation of biliary stricture u/s t,tube cholengiography if present ercp ercp ptc ptc ct ct cholengiography cbd
post operative stricture about 15% of injuries recognized at the time of operation and 85% of cases declares it self post operatively by 1- profuse and persistent leakage of bile through the drainage or bile peritonitis if no drainage 2- deepening obstructive jaundice bismuth classification of bile duct injury type 1 low cbd injury .stump >2cm type II middle common hepatic duct stump <2 cm type III---hilar confluence of rt and lf duct intact type IV rt and lf duct separated type V involvement of intra hepatic ducts
treatment in debilitating pt need drainage of bile either by pass per coetaneosly catheter to intrahepatic duct.or a stent pass through the duct trough ercp. after improvement of general condition of pt a definitive procedure can do. in benign stricture or duct transaction roux-en-y choledochjejunostomy. Malignat stricture balloon dilatation and insertion of stent is acceptable. Primary seclorosing cholengitis ITS CHRONIC FIBROTIC INFLAMATORY CONDITIONS OF UNKNOWN ORIGIN INVOLVE BOTH INTRA AND EXTRAHEPATIC BILIARY DUCT and may involve g.b and pancreas Its associated with inflammatory bowel ds in 50 -70 %,its premalignant condition to bile duct carcinoma .
Treatment difficult no surgery benefit because involve intra and extra hepatic ducts Usually treat with a.b vitamin k, cholestyramin, steroid and azathyoprine but with little benefit. Repeated dilatation of stricture may be helpful many pt go to liver cirrhosis and liver failure and need liver transplantation.
Carcinoma of Carcinoma of g. Rare condition main etiological factor are g.s .calcification of g.b ,and infection may promote carcinoma Metastasis easly to the liver by direct extension ,seeding to the peritoneal cavity ,and neural plexus. Investigation us. c/t scan and per coetaneous biopsy to confirm histological examination Cf Cf --same biliary colic and cholecystits .late sign jaundice ,palpable mass g.b b
Treatment if not invade serosa cholecystectomy enough. but if invade liver and hilar l.n prognosis poor 5% only 5year survival .