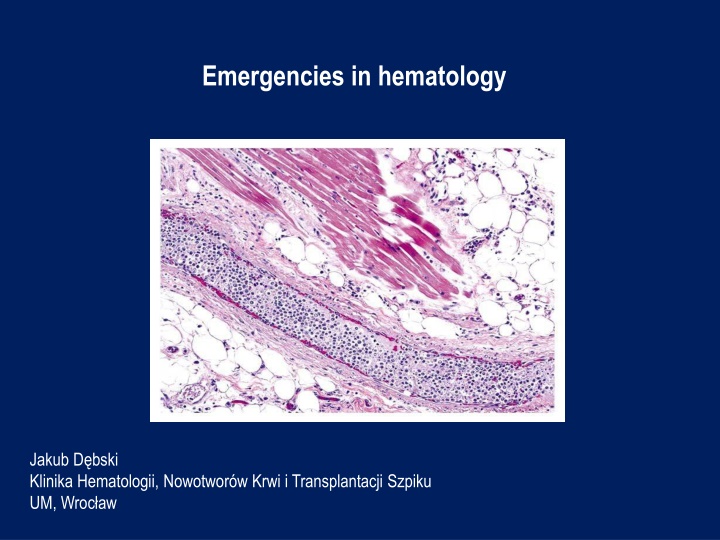
Emergencies in hematology
A 59-year-old patient with chronic lymphocytic leukemia presented with pneumonia and disease progression. Refusing chemotherapy, he developed severe pneumonia and worsening symptoms. Laboratory tests revealed critical values for leukocytes, hemoglobin, and thrombocytes, along with abnormal biochemistry results. This case requires urgent, comprehensive management to address the patient's complex condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Emergencies in hematology Jakub D bski Klinika Hematologii, Nowotwor w Krwi i Transplantacji Szpiku UM, Wroc aw
Patient 1 Interview: 59-year-old patient with chronic lymphocytic leukemia diagnosed in 2009 in stadium - Rai II, Binet B was transferred from the Internal Medicine Department to the Department of Hematology for the treatment of pneumonia and significant progression of the disease. The patient who was previously untreated hematologically, did not agree to the proposed chemotherapy during several visits in the outpatient clinics - the last visit on 8.01.2014. In March 2015, he was hospitalized in the Surgery Unit due to phlegmon of the left thigh. Then we found: leukocytosis 800 G / l, osteolytic lesions of left thighand pelvic bones , and in the performed on 17.03.2015 ultrasound examination of the abdominal cavity - hepatosplenomegaly with significantly enlarged lymph nodes, the largest with dimensions of 85 x 24 mm. The patient was advised to report urgently to the Hematology Clinic, but he did not. For about 3-4 days he had been observing cough, weakness, fever up to 40 C. Hospitalized in the Internal Medicine Unit between 29-30.04.2015 , in which he has been diagnosed with right-sided pneumonia with severe course and progression of untreated chronic lymphocytic leukemia.
Patient 1 At the reception on 30.04.2015: very severe condition, ECOG-3/4, drowsy, in a simple logical contact, conscious, aware, he reported a worsening of vision. In the physical examination: cachectic, right-sided rattling and crackling, left-sided crackles, RHA, tachypnoe 22 /min, abdomen arched above the chest level, soft, tender, without peritoneal symptoms, hepatosplenomegaly, numerous lymph node packages palpable through the abdominal wall, lymph nodes - cervical, axillary, inguinal enlarged up to 2-3 cm in diameter, organized in packets, numerous scars and skin cavities of the left lower leg due to the phlegmon (cured).
Patient 1 Peripheral blood morphology: WBC 982.77 10*3/uL [4-10] , IG% 0.3 % , NEUT% 1.6 % [40-75] , LYMPH% 89.4 % [25-45] , MONO% 9 % [2-12] , EO% 0 % [1-6] , BASO% 0 % , NRBC% 0 % , IG# 2.72 10*3/uL , NEUT# 14.99 10*3/uL [1.6-7.5] , LYMPH# 878.61 10*3/uL [1-4] , MONO# 88.9 10*3/uL [0.08-1.2] , EO# 0.07 10*3/uL [0.04-0.6] , BASO# 0.2 10*3/uL [0-0.1] , NRBC# 0.41 10*3/uL , RBC 2.06 10*6/uL [4.5-5.9] , HGB 5.8 g/dL [14-18] , HCT 19.1 % [37-53] , MCV 92.7 fL [81-98] , MCH 28.2 pg [26-34] , MCHC 30.4 g/dL [31-37] , RDW-SD 63.2 fL [37-54] , RDW-CV % 18.9 % [11-16] , PLT 51 10*3/uL [130-400] , PDW 12.4 fL [9-17] , MPV 10 fL [9-13] , P-LCR 28.2 % [13-43] .
Patient 1 In laboratory tests: In peripheral blood morphology Leukocytes 982.77 G / l, Hemoglobin 5.8 g / dl, Thrombocytes 51 G / l,? Procalcitonin 36.02 ng / ml, SaO2 82-84%, Biochemistry Increased level of glucose, CRP, LDH, urea, uric acid, ASPAT, ALP, total and direct bilirubin, magnesium, fibrinogen, D-dimers Decreased level of potassium, total protein, albumin What should be the further management of the patient?
Patient 1 The course of treatment: The patient was monitored, hydrated, and an urgent leukapheresis was performed followed by the first cycle of CVP (cyclophosphamide, vinblastine) chemotherapy in fractionated doses along with intravenous corticosteroids. RBC concentrate was transfused. In addition, broad-spectrum antibiotics and supportive care were used, achieving in the next days of stay an improvement in the general condition of the patient, along with moderate cytoreduction and a significant decrease in inflammation parameters. Due to the rebound of leukocytosis on 8.05.2015, another leukapheresis procedure was performed and the second and third CVP chemotherapy courses were implemented on 8.05.15 and 28.05.15, followed by further cytoreduction and moderate reduction of the size of the lymph nodes, liver and spleen. Because of insufficient response achieved after the 3 cycles of CVP, the therapeutic protocol was changed to FC-R (fludarabine, cyclophosphamide, rituximab), the first cycle of which was introduced with good tolerance.
Patient 1 Leukapheresis - a method of selective mechanical purification of plasma from morphotic elements - leukocytes (granulocytes, monocytes, leukemic blasts, CD34 + peripheral blood stem cells) using a separator.
Hyperleukocytosis Definition: leukocytes > 100 G / l It leads to complications: LS - leukostasis syndrome DIC disseminated intravascular coagulation TLS - tumor lysis syndrome The risk of complications depends on the biology of leukemic cells. Epidemiology: - AML - acute myeloid leukemia (10-20%) - subtypes M4, M5, microgranular variant M3 - ALL - acute lymphoblastic leukemia (10-30%) - T-cell subtypes, males, infants, 10-20 years of age (rarely leukostasis syndrome) - BL - lymphoma / Burkitt's leukemia - mainly TLS - CLL - chronic lymphocytic leukemia symptomatic > 400 G / l (rarely leucostatic syndrome) - CML - chronic myeloid leukemia - mainly in the blast crisis phase
Leukostasis syndrome - symptomatic hyperleukocytosis (clinical concept, not laboratory) - disturbances of blood flow and tissue perfusion as a result of accumulation of leukemic cells in the lumen of microcirculation vessels, often with activation of coagulation - most often affects the lungs (30%) and CNS (40%) Symptoms: - dyspnoea, hypoxia, diffuse vesicular hemorrhage, acute respiratory failure (ARDS) - visual impairment, optic nerve edema, retinal hemorrhages - disturbances of consciousness, dizziness, tinnitus, drowsiness, headache, delirium, coma, focal neurological deficits, intracranial hemorrhage - myocardial ischemia / ACS - acute limb ischemia - renal vein thrombosis, exacerbation of preexisting renal failure - priapism - intestinal infarction - fever (due to cytokine release or associated infection) - progression of respiratory distress sometimes in patients after the start of chemotherapy, (acute lysis pneumopathy)
Leukostasis syndrome In laboratory tests: pseudohypoxemia pseudohypoglycemia pseudohyperkalemia hypocalcaemia hyperphosphatemia hyperuricaemia lactic acidosis DIC features - about 40% TLS features - about 10%
Leukostasis syndrome Treatment: - urgent leukapheresis 2 procedures with an interval of 12-24 hours Indications for a leukapheresis: Diagnosis Symptomatic hyperleukocytosis (G/l) 50 150 150 500 No Asymptomatic hyperleukocytosis (G/l) 100 300 No No No AML ALL CML CLL APL
Leukostasis syndrome Treatment: - cytoreduction: hydroxycarbamide 50-100 mg / kg, usually 2-4 g / day, reduction in the value of leukocytosis by 50-80% within 24-48 hours - chemotherapy inducing remission - implemented when leukocytes < 50 G / l - adequate hydration and prophylaxis of tumor lysis syndrome - management of the coexist. intravascular coagulation syndrome - RBC concentrate transfusions - cautiously, slowly during or after the leukapheresis procedure - Platelet concentrate transfusions - maintenance of PLT level > 20- 30 G / l - antibiotic therapy - glucocorticoids
Leukostasis syndrome Contraindications to leukapheresis: - acute promyelocytic leukemia - cardiorespiratory insufficiency - severe cardiac diseases - severe coagulation disorders
Disseminated intravascular coagulation (DIC) - 10-15% pts with generalized tumors, 15% with leukemia - generalized activation of coagulation with fibrinolysis disorders + coagulopathy with consumption - in the clinical presentation: bleeding (60%) and thrombotic complications - 3 types of DIC accompanying tumors: procoagulant, hyperfibrinolytic, subclinical - diagnosis - serial analysis of platelet counts, PT and aPTT coagulation times, fibrin degradation markers: fibrin monomers, FDP, D-dimers, fibrinogen concentration
Disseminated intravascular coagulation (DIC) Management: - treatment of the underlying disease - transfusions of blood products: RBC concentrate - when there is a significant loss of blood FFP 10-15 ml / kg - active bleeding and elongation > 1.5-fold aPTT or PT FFP 15 ml / kg every 12-24 h or cryoprecipitate 1 unit / 10 kg every 24 h - active bleeding and fibrinogen < 1.0 g / l Platelet concentrate 1-2 U / kg - PLT < 20 G / l or PLT < 50 G / l + hemorrhagic diathesis - heparin (controversial) - should be considered in cases with predominant thrombotic symptoms - fibrinolysis inhibitors - tranexamic acid 10-15 mg / kg in DIC with enhanced fibrinolysis - in acute promyelocytic leukemia - DIC with hyperfibrinolysis, life-threatening hemorrhagic complications in about 5% (65% intracranial bleeding / 32% pulmonary bleeding) required application of ATRA (all-trans retinoic acid) or ATO (arsenic trioxide)
Tumor lysis syndrome (TLS) - life-threatening metabolic syndrome resulting from the rapid breakdown of cancer cells - high proliferative activity and high chemosensitivity of the tumor - spontaneous form - Burkitt's lymphoma, acute leukemia with high hyperleukocytosis - induced form - acute leukemia (ALL > 100 G / l, AML > 50 G / l), Burkitt's lymphoma, lymphoblastic lymphoma - renal failure increases the risk of TLS - metabolic disorders - hyperkalemia, hyperphosphatemia, hyperuricemia, hypocalcaemia, metabolic acidosis - symptoms - acute renal failure, arrhythmias / sudden cardiac death , hypotension, heart failure, convulsions, neuromuscular hyperactivity
Tumor lysis syndrome (TLS) Management: 1. prophylaxis - hydration 3 l / m2 / 24 h 0.9% NaCl + allopurinol 600- 900 mg / 24 h + eventually leukapheresis 2. treatment - diuresis forced by a loop diuretic > 3 l / 24 h, hourly 100 ml / h + allopurinol 500 mg / m2 / day - in the case of severe hyperuricaemia - rasburicase (recombinant xanthine oxidase) 0.2 mg / kg / day i.v. - hemodialysis in the development of acute renal failure - correction of electrolyte disturbances
Hypercalcemia - increased total calcium concentrations > 2.6 mmol / l (10.5 mg / dl) or ionized calcium > 1.25 mmol / l (5 mg / dl) - in the case of protein disorders (hypoproteinaemia, hypoalbuminaemia): calculation corrected calcium concentration (mg / dl) = [measured calcium concentration (mg / dl) - albumin concentration (g / dl)] + 4 - in hyperproteinemia - possible spurious hypercalcemia The most common causes are: - increased osteolysis in plasma cell myeloma - lymphomas and leukemia - paraneoplastic syndrome or severe osteolysis (PTH- independent) or production of 1,25(OH)2D3 - bone tissue neoplasms, bone metastases - primary hyperparathyroidism - overdose of vitamin D3 - persistent immobilization - thiazide diuretics, theophylline - hyperthyroidism - adynamic bone disease in dialysis patients
Hypercalcemia Mild hypercalcemia < 3.0 mmol / l (12 mg / dl) - asymptomatic Moderate and severe hypercalcemia 3.0 - 3.75 mmol / l (12-15 mg / dl) and rapidly increasing - hypercalcemic syndrome: 1. kidney problems - polyuria, hypercalciuria (nephrolithiasis, nephrocalcinosis) 2. gastrointestinal symptoms - lack of appetite, nausea, vomiting, constipation, gastric / duodenal ulcer, pancreatitis, cholelithiasis 3. cardiovascular symptoms - arterial hypertension, tachycardia, arrhythmia, hypersensitivity to digitalis glycosides 4. neuromuscular symptoms - muscle weakness, weak tendon reflexes, transient facial muscle paralysis 5. CNS symptoms - headache, depression, orientation disorders, drowsiness, coma 6. dehydration In a very severe hypercalcemia > 3.75 mmol / l (15 mg / dl) - hypercalcemic crisis: disturbances of consciousness, nausea, vomiting, abdominal pain, arrhythmias, dehydration, death. ECG - prolongation of the PQ interval, QT shortening, wide T wave, sometimes the Osborn wave
Hypercalcemia Management: - abundant hydration - 3-5 liters / day (~ 3 l / m2 / day) 0.9% NaCl - forced diuresis with furosemide 20-40 mg iv, diuresis: 150-200 ml / h - reducing the calcium release from bones - calcitonin 100 UI 2-4 times a day iv or bisphosphonates (eg. pamidronate 60-90 mg / 2 h iv or zoledronate 4 mg / 15 min iv) or denosumab - inhibition of calcium absorption from the gastrointestinal tract - glucocorticosteroids (eg. hydrocortisone 100 mg iv every 6 h) - in severe cases hemodialysis In chronic tumor hypercalcemia in addition: - mitramycin 25 ug / kg for 4-6 h i.v. or - gallium nitrate 100-200 mg / m2 for 24 hours for 4-5 days
Superior vena cava syndrome (SVCS) - syndrome of symptoms caused by impeding blood flow from the superior vena cava to the right atrium of the heart - 2-4% of patients with lung cancer and 2-4% with lymphoma The most frequent causes: - narrowing of the superior vena cava 1. external pressure + tumor infiltration of the vein wall - lung cancer (60-80%), lymphoma (10-15%), metastasis of breast cancer, mediastinal germ cell tumors, thymomas 2. non-neoplastic causes - aortic aneurysm, chronic mediastinitis - superior vena cava thrombosis - a catheter or secondary mediastinal tumor - right atrial tumor (rare)
Superior vena cava syndrome (SVCS) Symptoms: - swelling, erythema or bruising of the face - conjunctival hyperemia - swelling of the upper limbs - symptoms associated with increased intracranial pressure: headache and dizziness, visual disturbances, convulsions - permanent distention of the jugular veins and positive Pemberton s sign - dyspnea - hoarseness - difficulty in swallowing - stridor The chest CT scan is the test of choice to diagnose SVCS. Chest X-ray is normal in 5-15% of cases.
Superior vena cava syndrome (SVCS) Symptomatic treatment: - dexamethasone 16-32 mg / d i.v. for 7 days, then dose reduction - control of dyspnea - morphine, midazolam, oxygen therapy - loop diuretic (eg. furosemide) - low molecular weight heparin - prophylactic or curative Causative treatment: - urgent irradiation of the mediastinum - in the majority of cancers, the treatment of choice - chemotherapy - for chemosensitive cancers: lymphomas, lung cancer, germ cell tumors - introduction of the stent into the superior vena cava (removal of symptoms in > 75% of patients within 48 -72 h after surgery) - in the case of thrombosis - also consider thrombolysis
Differentiation syndrome in acute promyelocytic leukemia - life-threatening complication of the induction of acute myeloid leukemia M3 (promyelocytic) after application of ATRA or ATO - occurs in up to 25% of patients within 7-12 days of starting treatment - pathomechanism is not known, probably cytokine-related - symptoms: fever, increasing dyspnea, peripheral edema, skin rash, lung infiltration, fluid in the pleural cavity and pericardium, hypotension, renal insufficiency - risk increased by leukocytosis > 50 G / l - treatment: dexamethasone 2 x 10 mg iv until the symptoms disappear, sometimes dialysis is necessary and respiratory therapy - in patients with severe organ-related complications - temporary withdrawal of ATRA or ATO - mortality is around 1%
Neutropenic fever - neutropenia is the most common complication of anticancer treatment, it results from the myelotoxic action of chemo-radiotherapy or bone marrow infiltration by tumor cells - neutropenic fever - 10-50% of patients with solid tumors, > 80% with hematological malignancies Definition of neutropenic fever (febrile neutropenia): 1. oral temperature 38.3 C in single measurement or 38 C persistent for 1 hour 2. neutrophil count < 500 / ul or predicted decrease to < 500 / ul in 48 hours Patients with NF rarely have local infection or they are weakly expressed. Most often, bacterial infections (Gram +> Gram-), less often fungal and viral. Blood-borne infection - 13-60% of patients, mortality 12-42%. The most serious forms of infection are: pneumonia, neutropenic enteritis, septic shock.
Neutropenic fever Management: - broad-spectrum, wide-spectrum empiric antibiotic therapy, in patients at high risk of complications and death: carbapenem or piperacillin with tazobactam or ceftazidime or cefepime iv - addition of antifungal medication (eg. fluconazole iv) - microbiological tests - identification of the pathogen responsible for infection is successful in 20-30% of patients - use of granulocyte growth factors G-CSF or GM-CSF, if the patient did not receive them as a primary or secondary prophylaxis Regular assessment of the patient's condition, effectiveness of antibiotic therapy, development of complications every 24-48 hours is mandatory. In case of improvement or identification of an infectious agent - de-escalation of antibiotic therapy.
Prophylaxis in afebrile patients with neutropenia 1) a sanitary regime, hand and cough hygiene, sometimes patient isolation 2) prophylactic use of fluoroquinolone (ciprofloxacin, levofloxacin) - only in high-risk patients 3) prophylactic use of antifungal drugs (azoles, echinocandins) and antivirals (aciclovir) - only in patients undergoing allo-HCT and inducing remission chemotherapy in acute myeloid leukemia 4) prophylactic use of cotrimoxazole in patients with risk factors for Pneumocystis jiroveci infection - purine analogs, corticotherapy > 1 month 5) prophylaxis with G-CSF (filgrastim, lenograstim ) or GM-CSF (molgramostim, regramostim, sargramostim): - primary - recommended already during the first cycle of chemotherapy, when the risk of developing febrile neutropenia > 20%, to consider also in the case of intensive chemotherapy - secondary - recommended in patients with complications associated with neutropenia that occurred after the first chemotherapy cycle, and reducing the doses of cytotoxic drugs or delaying their administration may affect overall survival 6) avoidance of prolonged environmental contact a high concentration of fungal mold spores (constructions, old and neglected buildings)