Diabetes and Its Management in Students
Diabetes is a chronic condition characterized by high blood sugar levels. This article discusses the management and safety of students with diabetes, highlighting the types and classifications of diabetes, differences between Type 1 and Type 2 diabetes, and the presentations of diabetes. It emphasizes the importance of proper care to prevent serious health issues.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Management and Safety of students with Diabetes Kanika Ghai MD Division Director Pediatric Endocrinology Advocate Children s Hospital April 9, 2019
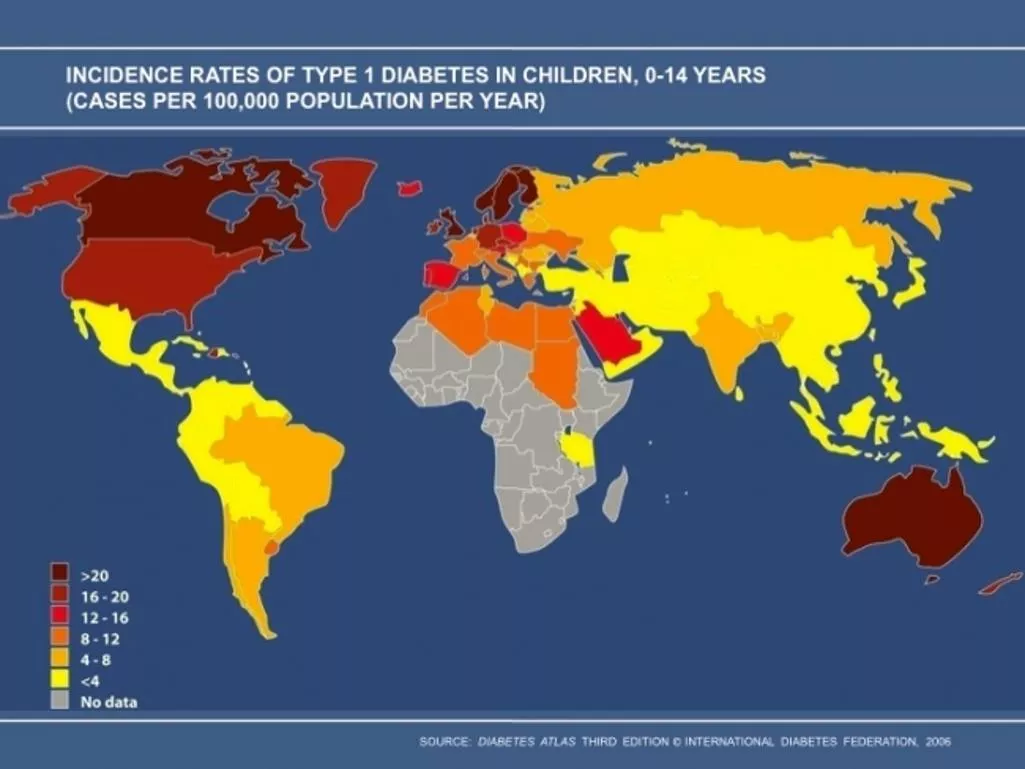
That continues to increase (Ann NY Acad Sci. 2008 December; 1150:1-13)
About 200,000 Americans under age 20 are estimated to have diagnosed diabetes approximately 0.25% of those under age 20 have diagnosed diabetes
What is Diabetes ? Diabetes is a chronic disease in which blood sugars are high People develop Diabetes because pancreas produce little or no insulin or the cells in the muscles, liver and fat do not use insulin properly High Blood Sugars ( Hyperglycemia) over the years can cause Serious Health Problems There is no Cure for Type 1 Diabetes
Classification of Diabetes Type -1 diabetes ( cell destruction, usually leading to absolute insulin deficiency) Immune mediated Idiopathic: ADM Type-2 diabetes( predominately insulin resistance with relative insulin deficiency) Other specific types (MODY, Genetic defects of insulin, diseases of pancreas, endocrinopathies, drug induced, infections, genetic syndromes.) Gestational Diabetes
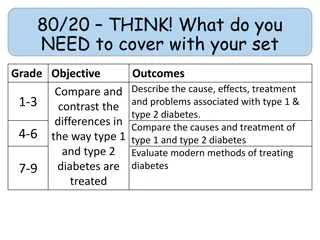
T1DM vs T2DM Type 1 diabetes mellitus Autoimmune in nature Requires insulin administration from time of diagnosis Type 2 diabetes mellitus Typically related to obesity May be treated with diet, oral medications or insulin therapy
Presentation of Diabetes Extremely variable May be asymptomatic found on routine screening May be critically ill requiring intensive care May initially present as diabetic ketoacidosis results from a lack of insulin body switches to burning fatty acids and producing acidic ketone bodies Vomiting, dehydration, deep gasping breathing and mental status changes are typical symptoms.
Signs & Symptoms of Diabetes Increased thirst Increased urination accidents daytime or nighttime Weight loss Abdominal pain Nausea / emesis Headaches Blurry vision
Diagnosing Diabetes Fasting Plasma Glucose (FPG) Glucose level after not having food or drink for at least 8 hours Result Normal - <100 mg/dl Prediabetes - 100 125 mg/dl Diabetes - >126 mg/dl
Diagnosing diabetes Random Plasma Glucose Glucose level at any time of the day when severe diabetes symptoms are present. Result Diabetes - > 200 mg/dl
Diagnosing Diabetes HgbA1c test measures average blood glucose for the past 2 to 3 months. Result Normal - less than 5.7% Prediabetes - 5.7% to 6.4% Diabetes - 6.5% or higher
Diagnosing Diabetes Oral Glucose Tolerance Test a two-hour test that checks your blood glucose levels before and 2 hours after consuming a high sugar drink Result Normal - less than 140 mg/dl Prediabetes - 140 mg/dl to 199 mg/dl Diabetes - >200 mg/dl
Treatment Insulin therapy : Most important Nutrition: High fiber, Less Free Sugar Active Lifestyle Frequent monitoring :Adjustments to correct high and low Blood sugars Prevention of High and Low blood sugars. Anticipate high or low Blood sugars from Blood sugar trends and intervene before they get abnormal
Blood glucose monitoring Allows one to determine the concentration of glucose in blood Helps guide management When to be done Before meals or snacks Before bedtime With changes in insulin doses Before activity When symptomatic Should be performed on finger-tip
CONVENTIONAL THEARPY Insulin Effect AM AN EVE NIGHT B D HS B L Meals
MULTIPLE DOSE INSULIN REGIMENS Short acting insulin analog/regular + NPH Insulin Effect AM AN EVE NIGHT B D HS B L Meals
Multiple Dose Insulin Regimens Novolog/Humalog/Apidra/Reg + Lantus/ Levemir/UL Insulin Effect AM AN EVE NIGHT B D HS B L Meals
Insulin dosing plans Typical insulin plan at meal or snack Step 1: Assess carbohydrate intake Step 2: Check Blood sugar Step 3: Calculate Food Dose/Carbohydrate dose. Step 4: Calculate Correction dose Step 5: Calculate Total Insulin Dose : Food dose + Correction dose Food intake: Ham sandwich, apple, glass of milk, Blood sugar: 262 Carbohydrate Intake =(15gms x 2+15gms+15 grams) = 60 grams Dose = 60/15 (4 units)+ 262-130/60 (2.2 units) Dose given = 6 units
Glucose sensors 3 parts: 1. Sensor 2. Transmitter 3. Receiver
Three Day Continuous Glucose Monitor
Caring for a child with diabetes A lot of a child s diabetes cares will take place at school Illinois has in place the Care of Students with Diabetes Act Provides requirements school must meet in regards to care of diabetes Difficult for many schools to have required training and personnel available A partnership between nurse, students, parents and medical home
Effective Diabetes Management at School Goal: Keep Blood sugar levels within target range determined by health care team Assist Student in performing Diabetes care tasks Designating Trained Diabetes Personnel
How to plan Effective management in School Setting Assemble health care team Review Federal Laws Assemble Student s health care plan Diabetes Management plan (health care team) Individualized health care plan ( school nurse) Emergency care plans(school nurse) Prepare Student s education plan Train School Personnel Diabetes Management Training resources
Review Federal Laws Section 504 of the Rehabilitation act of 1973 (section 504) American with Disabilities Act of 1990 (ADA) Individuals with Disabilities Education act (IDEA)
Diabetes Care Plan Also known as a diabetes medical management plan (DMMP) Provides direction for diabetes cares at school Per Diabetes Care Act a DMMP is required: upon enrollment, as soon as practical following a student's diagnosis; or when a student's care needs change during the school year. Parents shall be responsible for informing the school in a timely manner of any changes to the diabetes care plan and their emergency contact numbers.
Diabetes Care Plan Provides information on: Monitoring of blood glucose Dosing of insulin Authorization for insulin use Treatment of hypoglycemia Authorization for glucagon use Treatment of hyperglycemia Use of insulin pump Physical activity and sports Nutrition
Train School Personnel Level 1Training: All school personnel Level 2 Training: school personnel who have responsibility for the student Level 3: School staff designated as trained Diabetes personnel
Help students lmplement Effective Diabetes management Check BG Plan Disposal of sharps Recognize and Rx low BG Recognize and Rx high BG Administer insulin and/or other Diabetes medication Plan for emergency Plan Individualized meal plan Plan for special events, field trips Promote Regular physical activity Deal with emotional and social issues
Hypoglycemia Too much Insulin Missing or delaying meals or snacks Not eating enough food (carbohydrates) Getting additional, intense, unplanned physical activity Being ill particularly with gastrointestinal illness Hypoglycemia is not always preventable Not every student can recognize hypoglycemia
Checklist for Hypoglycemia Mild/moderate : Oral glucose and recheck BG Student should not be left alone or sent anywhere alone or with another student Severe: Glucagon use Position child to side Do not feed orally Call 911 Administer Glucagon Call parents /guardian Stay with student
Checklist for Hyperglycemia Check BG and repeat every 2 hours Check urine ketones Give insulin correction dose Give Extra fluids (sugar free) Allow unrestricted access to restroom Restrict participation in physical activity per DMPP Notify parents Pump: Check if pump is connected properly For suspected pump failure give insulin via injection
Classification of Diabetes Mellitus Nelson Essentials of Pediatrics, 7th Edition