Comprehensive Guide to Gynaecological Malignancies and Care
Explore the essentials of gynaecological malignancies, including endometrial cancer, cervical carcinoma, ovarian cancer, vulval cancer, and more. Learn about government waiting time pledges, diagnostic procedures, treatment options like surgery, radiotherapy, and chemotherapy, referral networks, the role of Cancer Nurse Specialists, psychosexual issues, financial support, and classification of ovarian malignancies. Stay informed and empowered in managing gynaecological cancers.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
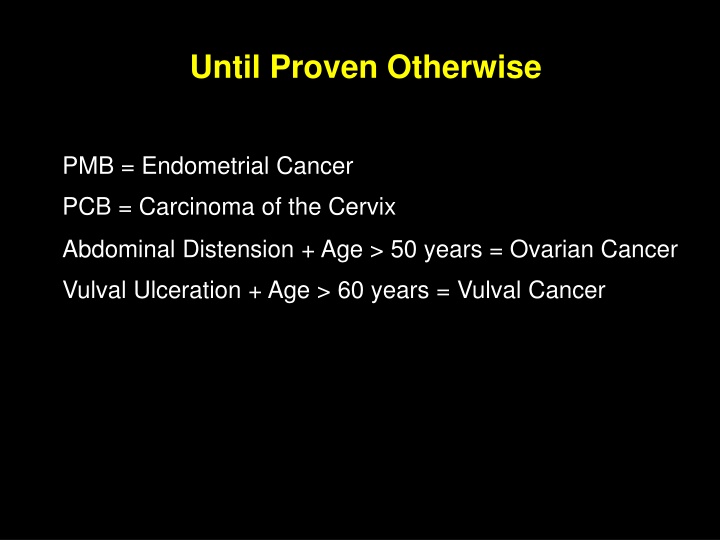
Until Proven Otherwise PMB = Endometrial Cancer PCB = Carcinoma of the Cervix Abdominal Distension + Age > 50 years = Ovarian Cancer Vulval Ulceration + Age > 60 years = Vulval Cancer
Government Pledges on Waiting Times Maximum Duration of Waiting: 62 DAYS Urgent Referral for ? Cancer to 1st Px 31 DAYS Date of Decision to Treat to 1st Px (DTT) 31 DAYS Subsequent Surgery or Radiotherapy or Anti-Cancer Drug Regimen 14 DAYS Suspected Cancer Symptoms to Seeing a Specialist
Gynaecological Malignancy Growth without control local Invasion distant Diagnosis Biopsy remove Treatment destroy
Surgery Radiotherapy Chemotherapy
MDT GCLN
Referral to the Network(Central) MDT Ovary/Peritoneum Uterine Cervix Vagina Vulva Recurrent cancer
Role of CNS(Cancer Nurse Specialist) All woman with a gynaecological cancer should have access to a CNS and is identified as the Key Worker CNS facilitates the woman and her carer s needs throughout the cancer pathway from diagnosis Provision of advice, support and information. Receptive to a full range of social, physical, psychological, cultural, sexual health and spiritual needs. Link professional who can help patients through the system. Co-ordinator of care and services Works closely with surgeons, oncologists, radiotherapists and other professionals Nurse Led Clinics Breaking bad news clinics Cancer Follow up clinics Holistic Assessment Transition of care on discharge to GP
Psychosexual Issues HRT and menopausal information Lymphoedema
Finance Support agencies Local and national support groups Hospice Care
Classification of Ovarian Malignancy Epithelial origin Germ cell origin Stromal cell origin
Tumour Markers in Serum CA125 FP Epithelial Ovarian Malignancy Yolk sac tumour Trophoblastic tumours choriocarcinoma HCG Alkaline phosphatase Lactate dehydrogenase Dysgerminoma FSH + LH Granulosa cell tumour FP + HCG Embryonal carcinoma, Polyembryoma
Specific Histopathological Features of Gynaecological Tumour Granulosa cell tumour Call Exener Body Schiller Duval Body Yolk sac tumour Serous papillary cystadenocarcinoma ovary Psammoma Body Reink crystalloids Leydig cell tumour ovary
Calculation of the Risk of Malignancy Index (RMI) for a Pelvic Mass A RMI calculation of greater than 200 indicates a high suspicion of ovarian malignancy. CA125 measurement A Menopausal status Premenopausal Postmenopausal (amenorrhoea >= 1 year, or over 50 years and post hysterectomy) B Score 1 Score 3
Ultrasound Score Multilocular lesion Solid areas Bilateral lesions Ascites Intra abdominal metastases If none or one of the above is present score 1, if 2-5 of above score 3 C
RMI = A*B*C Young premenopausal patient with a unilateral, unilocular cyst on scan with a CA125 of 30. RMI =30*1*1=30 c.f. Postmenopausal patient with bilateral solid ovarian tumour and CA125 of 300. RMI=300*3*3=2700.
SINGLE BEST ANSWER QUESTIONS (SBAs) Author Mr S J Duthie Theme Gynaecological oncology Domain Treatment 1 ITEM 1 Which one of the following is the dose limiting toxicity of cis- Platin? Options A Central neurotoxicity B Myeolotoxicity C Nephrotoxicity D Ototoxicity E Peripheral neurotoxicity ANSWER C
ITEM 2 Which one of the following is the dose limiting toxicity of carbo- Platin? Options A Central neurotoxicity B Myeolotoxicity C Nephrotoxicity D Ototoxicity E Peripheral neurotoxicity ANSWER B ITEM 3 Which one of the following is the dose limiting toxicity of Oxaliplatin? Options A Aplastic anaemia B Haemorrhagic cystitis C Peripheral neuropathy D Pulmonary fibrosis E Retinopathy ANSWER C
SINGLE BEST ANSWER QUESTIONS (SBAs) Author Mr S J Duthie Theme Domain Genetics 1 Gynaecological oncology ITEM 1 Which one of the following is the single most correct description of the genetic transmission of Lynch Syndrome (Hereditary non-polyposis colon cancer syndrome)? Options A Autosomal dominant with a high penetrance of 90% B Autosomal dominant with a low penetrance of 20% C Autosomal dominant with a moderate penetrance of 50% D Autosomal recessive with a high penetrance of 90% E Autosomal recessive with a low penetrance of 20% ANSWER A
SINGLE BEST ANSWER QUESTIONS (SBAs) Author Mr S J Duthie Theme Domain Genetics B Gynaecological oncology ITEM 1 Women with a mutation in the BRCA1 gene have an increased lifetime risk for fallopian tube/ovarian cancer of approximately which one of the following? Options A 30% B 40% C 50% D 60% E 70% ANSWER D
ITEM 2 Peutz-Jeghers Syndrome is an autosomal dominant condition with a penetration of which one of the following? Options A 10% B 25% C 75% D 95% E Variable ANSWER D
SINGLE BEST ANSWER QUESTIONS (SBAs) Author Theme Gynaecological oncology Domain Genetics 1 Mr S J Duthie ITEM 1 In women with sporadic ovarian cancer, a co-existing endometrial tumour occurs in approximately which one of the following? Options A B C D E 0.1 % 2 % 4 % 9 % 10 % ANSWER B
ITEM 2 In women with ovarian cancer associated with Lynch Syndrome (Hereditary non- polyposis colon cancer syndrome) a co-existing endometrial tumour occurs in approximately which one of the following? Options A B C D E 5 % 10 % 15 % 20 % 40 % ANSWER D Reference Beirne J.P., Irwin G.W., McIntosh S.A., Harley I.J.G. and Harkin D. P. The Molecular and Genetic Basis of Inherited Cancer Risk in Gynaecology. TOG
SINGLE BEST ANSWER QUESTIONS (SBAs) Author Theme Gynaecological oncology Domain Granulosa cell tumour 1 Mr S J Duthie ITEM 1 In a postmenopausal woman with a granulosa cell tumour of the ovary, the serum level of which one of the following is the most likely to be increased? Options A B C D E Cortisol Follicle stimulating hormone Growth hormone Inhibin B Luteinising hormone ANSWER D
EXTENDED MATCHING QUESTIONS (EMQs) Author Mr S J Duthie Theme Gynaecological oncology Domain Endometrial Cancer risk factors Options A B C D E F G H I J Cigarette consumption Diabetes mellitus Early menarche High body mass index History of polycystic ovarian syndrome History of unopposed oestrogen therapy Hypertension Late menopause Nulliparity Use of barrier contraception
ITEM 1 A 60 year old nulliparous woman has been fast tracked to your clinic as her General Practitioner noted a 5 week history of postmenopausal vaginal bleeding. You review her history and observe that the woman reached her menarche at the age of 10 years and her menopause at the age of 53 years. The woman had tried to get pregnant in the past, underwent tests which showed that she had polycystic ovarian syndrome and there was a very limited response to ovulation induction. Subsequently, the woman used barrier methods of contraception. Shortly after menopause, the woman was given a prescription for hormone replacement therapy. Inadvertently, the woman received unopposed oestrogen for 2 months, developed irregular vaginal bleeding, the HRT was stopped, assessments at the PMB clinic were reassuring and the woman decided not to use any form of HRT again. The woman has mild hypertension, adult onset diabetes mellitus which is well controlled by dietary modification and an oral hypoglycaemic agent and she consumes 5 cigarettes daily. On examination, the woman has a body mass index of 48 kg/ m2 Pelvic examination shows that the uterus is bulky and histological examination of a pipelle biopsy of the endometrium shows adenocarcinoma of the endometrium. Which one of the factors in the list of options is the single most significant risk factor for endometrial cancer in this particular case? ANSWER D
EXTENDED MATCHING QUESTIONS (EMQs) Author Theme Domain Tumours 1 Mr S J Duthie Gynaecological disorders Options A B C D E F G H I J K L M N Benign cystic teratoma Borderline ovarian tumour Borderline serous tumour Brenner tumour Chocolate cyst Cyst of the corpus luteum Follicular cyst Granulosa cell tumour Krukenburg tumour Metastatic breast cancer Mucinous cystadenocarcinoma Ovarian fibroma Papillary serous cystadenocarcinoma Theca lutein cyst Each of the clinical scenarios listed below refers to non pregnant women with a pelvic mass. For each of the items choose the most likely diagnosis from the list of options given above. Each option may be used once, more than once or not at all. Each option may be used once, more than once or not at all.
ITEM 1 A previously healthy 23 year old woman complains of abdominal pain, abdominal swelling and tiredness. On clinical and radiological assessment the woman is found to have a solid pelvic mass with a diameter of 15 cm which is separate from a normal uterus, abdominal ascites and a left sided pleural effusion. The serum CA 125 is well within the normal range. ANSWER L ITEM 2 A 24 year old woman has undergone suction evacuation of the uterus for suspected molar pregnancy. Inspection of the products and histopathological examination confirm the diagnosis. The woman complains of abdominal pain and an ultrasound examination carried out 4 days postoperatively shows; Empty normal sized uterus, bilateral adnexal masses each of which has a diameter of 8 cm. The lesions are thin walled, cystic and do not appear to contain any solid elements. ANSWER N
EXTENDED MATCHING QUESTIONS (EMQs) Author Mr S J Duthie Theme Gynaecological Oncology Domain Tumour Histopathology 1 Options A B C D E F G H I J Barr body Call- Exner body Copper sulphate crystals Howell- Jolly body Kimmelstiel-Wilson lesion Lines of Zahn Psammoma body Reinke s crystals Schiller-Duval body Sternberg-Reed cells Select the single most correct term from the list of options for the histopathological findings in the gynaecological tumours described in the items below. Each option may be used once, more than once or not at all.
ITEM 4 A 45 year old woman underwent total abdominal hysterectomy bilateral salpingo- oophorectomy for suspected ovarian cancer. The woman had completed her family, was known to have a pelvic mass and her case had been discussed at a gynaecological multi-disciplinary team meeting. The operation specimen was examined in the pathology laboratory. The uterus was normal in size, the tubes appeared normal, the right ovary was normal in size and the left ovary contained an infiltrative mass with no obvious capsule. The lesion in the left ovary contained minute concentric lamellated calcified bodies visible using light microscopy. Select the term for this feature from the list of options. ANSWER G
EXTENDED MATCHING QUESTIONS (EMQs) Author Theme Domain Pelvic tumours 1 Mr S J Duthie Gynaecology Options A B C D E F G Benign cystic teratoma Choriocarcinoma Endometrioma Fallopian tube carcinoma Granulosa cell tumour Krukenburg tumour Metastasising melanoma H I J K L M Ovarian cancer Ovarian fibroma Placental site tumour Theca lutein cyst Uterine metastasising fibroid Uterine sarcoma The list of options contains tumours affecting the female genital tract. Each of the clinical scenarios listed below refers to a woman with a tumour affecting the genital tract. For each of the items choose the single most likely diagnosis from the list of options given above. Each option may be used once, more than once or not at all.
Options A B C D E F G Benign cystic teratoma Choriocarcinoma Endometrioma Fallopian tube carcinoma Granulosa cell tumour Krukenburg tumour Metastasising melanoma H I J K L M Ovarian cancer Ovarian fibroma Placental site tumour Theca lutein cyst Uterine metastasising fibroid Uterine sarcoma ITEM 1 You are called to the operating theatre by the surgical team who have just carried out emergency midline laparotomy on a 56 year old woman with a pelvic mass. The specialist trainee in Surgery has discussed the operation with his Consultant (not present) and they request you to attend. You observe that the woman has ascites, bilateral solid ovarian tumours which are not adherent to surrounding structures and peritoneal induration. The uterus is normal and the fallopian tubes are stretched over the ipsilateral ovarian tumours. You telephone your Consultant who is busy with an obstetric emergency. Your Consultant asks you to take multiple representative biopsies, send peritoneal fluid for cytological tests. close the abdomen, to return the woman to the gynaecology ward for postoperative care and arrange referral to the Gynaecological Multi- Disciplinary team. Three days later the Pathologist reports that histological diagnosis of the ovarian biopsies show malignant mucin containing signet cell rings. ANSWER F
Options A B C D E F G Benign cystic teratoma Choriocarcinoma Endometrioma Fallopian tube carcinoma Granulosa cell tumour Krukenburg tumour Metastasising melanoma H I J K L M Ovarian cancer Ovarian fibroma Placental site tumour Theca lutein cyst Uterine metastasising fibroid Uterine sarcoma ITEM 2 You are called to your Consultant s office as he is away and the Secretary wants you to look at a histopathology report that has just arrived. The report is on a hysterectomy specimen. Your Consultant had supervised another trainee one week previously to carry out total abdominal hysterectomy on a 40 year old woman of Afro-Caribbean origin who had a uterine fibroid, menorrhagia and who had completed her family. The pathology report states that there was an intramural fibroid with a diameter of 10 cm. There was a soft friable mass within the uterine fibroid and histological examination of the lesion showed local invasion, spindle cells and 10 mitoses per high- power fields ANSWER M
COLPOSCOPY EXAMINATION - ABNORMAL CIN1 untreated Repeat in 12/12 HR-HPV -ve Repeat in 36 months HR-HPV +ve Cytology -ve Repeat in 12/12 Cytology +ve Colposcopy referral HR-HPV -ve Repeat in 36 months HR-HPV +ve Cytology -ve Repeat in 36 months HR-HPV +ve Cytology abnormal Colposcopy referral
COLPOSCOPY EXAMINATION - ABNORMAL >=CIN2 Treatment Repeat in 6/12 HR-HPV +ve HR-HPV -ve Repeat in 36 months Cytology normal or abnormal Colposcopy referral
COLPOSCOPY EXAMINATION - ABNORMAL CGIN Treatment Repeat in 6/12 HR-HPV -ve Repeat in 12/12 HR-HPV +ve Cytology abnormal Refer to colposcopy. Complete 10-yr cytology follow-up Cytology negative Refer to colposcopy. If normal colposcopy, repeat in 12/12 12/12 repeat test HR-HPV +ve HR-HPV -ve Repeat in 36 months Cytology negative Refer to colposcopy. If normal colposcopy, repeat in 12/12 Cytology abnormal Refer to colposcopy. Complete 10-yr cytology follow-up
CGIN Glandular Premalignancy High grade / Low grade Most arise within 1cm of SCJ Co-exists with CIN No reliable screening method No specific colposcopic features Cone biopsy depth > 25mm
Precision Medicine Identify and understand molecular defect Determine presence Correct molecular defect
The End Thank you very much. S. J. Duthie