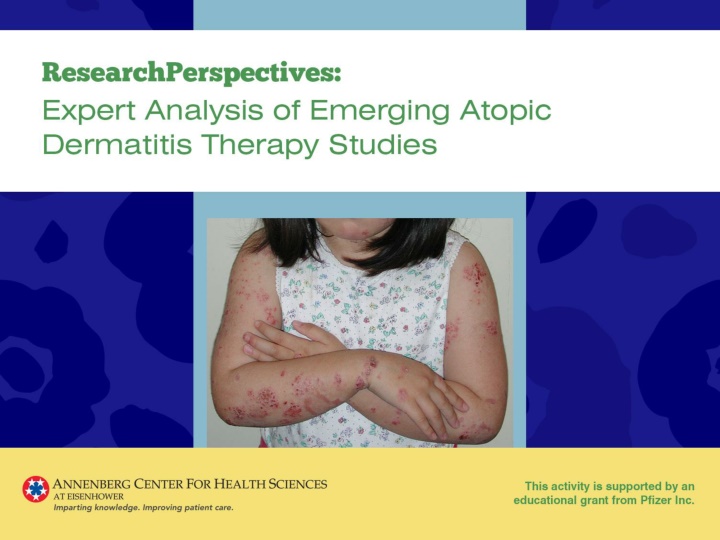
Comparative Analysis of Crisaborole Ointment and Dupilumab in Atopic Dermatitis
Crisaborole ointment, a nonsteroidal PDE4 inhibitor, demonstrated efficacy and safety in the treatment of atopic dermatitis in patients aged 2 years and older. Results from two phase 3 studies showed a significant improvement in disease severity with crisaborole compared to the vehicle. Treatment-related adverse events were mild-to-moderate, with application site burning/stinging being the most common. In comparison, Dupilumab, another treatment option, showed promising results in two phase 3 trials versus placebo for atopic dermatitis. Both treatments offer hope for patients with mild-to-moderate AD.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Efficacy and Safety of Crisaborole Ointment, a Novel, Nonsteroidal Phosphodiesterase 4 (PDE4) Inhibitor for the Topical Treatment of Atopic Dermatitis (AD) in Children and Adults Paller A, Wynnis T, Lebwohl M, et al. http://www.jaad.org/article/S0190-9622(16)30330-9/abstract
Study Design and Methods Crisaborole enhances cellular control of inflammation by inhibiting PDE4 leading to suppressed cytokine release 2 identically designed randomized, double-blind, vehicle- controlled phase 3 studies at 89 centers in the United States Patients age 2 years with mild-to-moderate atopic dermatitis with 5% treatable body surface area Randomized 2:1 to crisaborole or vehicle twice daily for 28 days Applied to all sites (except hair-bearing scalp) Primary objective: assess efficacy and safety of crisaborole with success defined as Investigator s Static Global Assessment (ISGA) score at day 29 of clear (0) or almost clear (1)
Results Summary Of the 1527 patients randomized, 1398 completed the study 12 patients in the crisaborole groups and 6 in the vehicle groups withdrew due to adverse events Significantly more crisaborole--than vehicle-treated--patients achieved the primary endpoint Study 301: 32.8% vs 25.4% Study 302: 31.4% vs 18.0% Significantly more crisaborole--than vehicle-treated--patients were clear or almost clear at study end Study 301: 51.7% vs 40.6% Study 302: 48.5% vs 29.7%
Results Summary (cont) Significantly more patients treated with crisaborole achieved improvement in erythema, exudation, excoriation, induration/papulation, and lichenification Patients treated with crisaborole achieved success in ISGA score as well as improvement in pruritus earlier than those treated with vehicle Treatment-related adverse events were infrequent and mild-to-moderate in severity in both groups Application site burning or stinging was the most common, and occurred in the majority on the first day with resolution within 1 day of onset
Two Phase 3 Trials of Dupilumab Versus Placebo in Atopic Dermatitis Simpson E, Bieber T, Guttman-Yassky E, et al. http://www.nejm.org/doi/pdf/10.1056/NEJMoa1610020
Study Design and Methods Dupilumab is a human monoclonal antibody against IL-4 receptor alpha 2 identically designed randomized, double-blind, placebo-controlled, parallel-group phase 3 studies at sites in North America, Europe, Asia Adults with moderate-to-severe atopic dermatitis for 3 years inadequately controlled with topical treatment Randomized 1:1:1 ratio to subcutaneous administration for 16 weeks of Dupilumab 300 mg weekly Dupilumab 300 mg every other week Placebo weekly Primary objective: assess the proportion of patients with an Investigator s Global Assessment (IGA) score demonstrating clear or almost clear skin with a 2-grade or more improvement from baseline to week 16
Results Summary 1379 patients randomized; 73 dupilumab and 86 placebo patients did not complete the study 18 in the dupilumab group and 24 in the placebo group withdrew due to an adverse event Significantly more dupilumab--than placebo-treated--patients achieved the primary endpoint SOLO 1: dupilumab every other week (38%), dupilumab every week (37%), and placebo every week (10%) SOLO 2: dupilumab every other week (36%), dupilumab every week (36%), and placebo every week (8%) Significantly more patients treated with dupilumab than placebo achieved improvement from baseline to week 16 of at least 75% on the Eczema Area and Severity Index (EASI) The proportion of patients was similar in the dupilumab weekly and every other week groups
Results Summary (cont) By week 2, improvement in pruritus was significantly greater with dupilumab Dupilumab significantly reduced patient-reported symptoms of atopic dermatitis and its effect on sleep, symptoms of anxiety or depression, and quality of life Fewer patients treated with dupilumab received rescue treatment Injection site reactions were more common in the dupilumab groups; most were mild or moderate Exacerbations of atopic dermatitis and most types of skin infections were more common in the placebo groups
Efficacy of Sodium Hypochlorite (Bleach) Baths to Reduce Staphylococcus aureus Colonization in Childhood Onset Moderate-to-Severe Eczema: A Randomized, Placebo-Controlled Cross-Over Trial Hon KL, Tsang YCK, Lee VEY, et al. http://www.tandfonline.com/doi/pdf/10.3109/09546634.2015.1067669
Study Design and Methods Bleach has antimicrobial activity against S. aureus, including MRSA Randomized, double-blind, placebo-controlled, crossover study at a single site Children and adolescents ages 4-18 years with moderate-to-severe atopic dermatitis Randomized 1:1 ratio to bleach 0.005% or placebo (water) 2-3 times weekly for 4 weeks followed by a 4-week washout period, then crossover treatment for 4 weeks Primary endpoint- change in S. aureus colonization at the right antecubital fossae and most severely infected or eczematous lesions before vs following treatment
Results Summary 40 patients were randomized and completed the trial, although nonadherence was noted in 14 Nonadherence was defined as bathing less than twice weekly, delayed follow-up after each treatment period, or use of an oral antibiotic S. aureus colonization was found in 80% and 85% of patients in the bleach and placebo baths, respectively, at baseline Reduced S. aureus growth was observed in 25% and 28% of bleach and placebo patients, respectively No significant effect on S. aureus resistance was observed
Results Summary (cont) A significantly greater reduction in the Scoring Atopic Dermatitis (SCORAD) index was observed with placebo Bleach baths conferred no significant efficacy benefit in measures of quality of life, skin hydration, and transepidermal water loss Bleach baths caused significantly greater reduction in topical corticosteroid use and topical antibiotic use Adverse events, primarily stinging and itch, did not differ between groups
Efficacy and Safety of Ustekinumab Treatment in Adults with Moderate-to-Severe Atopic Dermatitis Khattri S, Brunner PM, Garcet S, et al. http://onlinelibrary.wiley.com/doi/10.1111/exd.13112/full
Study Design and Methods Ustekinumab is a monoclonal antibody that blocks IL-12 and IL-23, thereby inhibiting Th1 and TH17/Th22 responses Randomized, double-blind, placebo-controlled, phase 2 study at a single US site Adults with moderate-to-severe atopic dermatitis inadequately controlled with conventional therapy Randomized 1:1 ratio to subcutaneous administration at weeks 0, 4, and 16 (with crossover at week 16) to Ustekinumab 45 mg or 90 mg (weight 100 kg vs >100 kg) Placebo Primary endpoint- 50% decrease from baseline in Scoring of AD (SCORAD50) at week 16
Results Summary 33 patients were randomized, with 21 completing the study through week 40 9 withdrew due to lack of efficacy (5 ustekinumab and 4 placebo) None discontinued due to an adverse event There was a profound and similar decrease in SCORAD from baseline through 40 weeks in both groups At week 16, 31% of ustekinumab and 19% of placebo patients achieved SCORAD50 Placebo- responses relatively flat between weeks 2 and 16 Ustekinumab- number of SCORAD50 responders increased through 20 weeks, decreased during weeks 16 through 28, then remained stable from weeks 32 to 40
Results Summary (cont) The SCORAD50 results suggest an optimal response 8 weeks after administration of ustekinumab Gene profiling showed a strong treatment effect with ustekinumab but not placebo by 4 weeks that increased through 32 weeks (16 weeks after last ustekinumab injection) Same treatment effect was observed with Th1, Th2, and Th17 14 patients experienced a total of 24 adverse events, all of which were mild or moderate There were no significant differences between groups in frequency of adverse events
Topical Tofacitinib for Atopic Dermatitis: A Phase IIa Randomized Trial Bissonnette R, Papp KA, Poulin Y, et al. http://onlinelibrary.wiley.com/doi/10.1111/bjd.14871/epdf
Study Design and Methods Tofacitinib is a Janus kinase-signal transducer and activator of transcription (STAT) pathway The study was a randomized, double-blind, vehicle-controlled, parallel group, phase 2a study at 5 sites in Canada Adults with mild-to-moderate atopic dermatitis with lesions covering 2%-20% of body surface area Randomized 1:1 to tofacitinib 2% or vehicle twice daily for 4 weeks Applied to all sites (except hair-bearing scalp) at a rate of 3 mg/cm2 Primary objective: assess percentage change from baseline in the Eczema Area and Severity Index (EASI) score at week 4
Results Summary 9 patients were randomized, with 65 completing the study 2 withdrawals due to an adverse event Mean percentage change from baseline to week 4 in the EASI total score was 81.7% for tofacitinib compared with 29.9% for vehicle Patients treated with tofacitinib experienced a more rapid response based upon the EASI, Physician s Global Assessment, and change from baseline in body surface area with significantly greater improvement in the tofacitinib group beginning at week 1 Improvement in pruritus was observed by day 2 with tofacitinib At week 4, the proportion of patients with a Physician Global Assessment of clear or almost clear for tofacitinib was 73% compared with 22% for vehicle Safety and local tolerability were generally similar for both treatments More adverse events were observed with the vehicle than for tofacitinib, although mild/moderate infection occurred in 6 tofacitinib and 3 vehicle patients
Efficacy of Omalizumab in Patients With Atopic Dermatitis: A Systematic Review and Meta-Analysis Wang HH, Li YC, Huang YC http://www.jacionline.org/article/S0091-6749(16)30615-7/pdf
Study Design and Methods Systematic search for randomized controlled clinical trials, comparative studies, and case series PubMed, MEDLINE, EmBase, and the Cochrane Library from inception through November 30, 2015 Omalizumab dosing regimens were divided into 2 groups 600 mg/month included 300 mg every 2 weeks or 150 mg every week <600 mg/month included 150 mg every 2 weeks or 300 mg every 3 weeks Clinical responses were defined as: Excellent: SCORAD reduction >50%, EASI reduction >75%, or IGA 0, or any improvement of 2-degree in IGA/modified IGA severity Satisfying: SCORAD reduction 25% to 50%, EASI reduction 25% to 50%, or a 1-degree improvement in IGA/modified IGA severity None: SCORAD reduction <25%, EASI <50%, or identical IGA severity Disease severity was defined as mild, moderate, severe
Results Summary 13 studies involving 103 patients were included in the analysis; 2 were clinical trials and 11 case series At baseline 60.5% had severe atopic dermatitis 76% had a history of allergic asthma 25% had total serum IgE levels <700 IU/mL; 43.4% had serum IgE levels >5000 IU/mL 66.7% were treated with 600 mg/month of omalizumab Clinical response: excellent 42.7%, satisfactory 25.2%, none or deterioration in 33.1%