Challenges and Solutions in Advance Care Planning
Advance care planning in medical offices faces difficulties due to lack of time, reluctance to discuss, inadequate knowledge, reimbursement issues, and lack of support. Research shows the impact of advance care planning on end-of-life care in elderly patients and highlights the benefits of following patients' wishes. The importance of addressing time constraints, improving understanding, and enhancing communication among physicians, care teams, patients, and families is emphasized. Strategies such as implementing advance directives and POLST, providing education, and promoting patient enrollment are key in overcoming these challenges.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
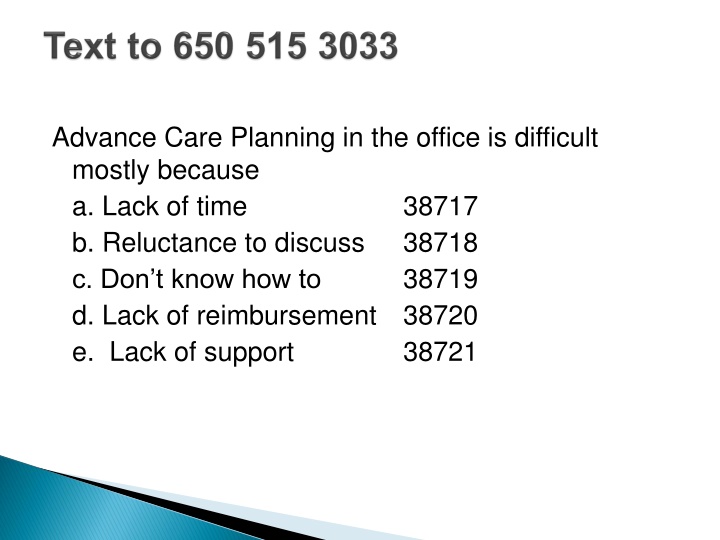
Advance Care Planning in the office is difficult mostly because a. Lack of time b. Reluctance to discuss c. Don t know how to d. Lack of reimbursement e. Lack of support 38717 38718 38719 38720 38721
RESEARCH The impact of advance care planning on end of life care in elderly patients: randomized controlled trial The impact of advance care planning on end of life care in elderly patients: randomized controlled trial Karen M Detering, respiratory physician and clinical leader1, Andrew D Hancock, project officer1, Michael C Reade, physician2, William Silvester, intensive care physician and director1 35 30 25 20 Wishes not folowed 15 Wishes followed 10 5 0 Intervention Control
Effects of POLST Effects of POLST
Lack of Time Lack of Understanding Needs, processes Reluctance to Discuss Physicians, care teams, patients, families Skill Needs System deficiencies
Initial 6 months 180 team interactions 120 attend Part 1 (Advance Directives) 46 attend Part 2 (POLST)
Initial 6 months 180 staff interactions 120 attend Part 1 (Advance Directives) 46 attend Part 2 (POLST) 29/46 attendees of Part 1 and Part 2 complete Advance Directive and/or POLST
Patient Identification through EMR Initial Education provided by MA MD Reinforcement Enrollment in Group session or Individual appointment
Patient Identification 70 yo; or 60 yo with chronic disease Initial Education Staff responsibility Offer Advance Health Care Directive information or POLST information
Engagement MD role Reinforce Need/Education Provide relevant personal clinical information
Must document the length of time of your visit within your note and state that >50% of the time was spent in counseling Then bill the time-based E/M (CPT) code (e.g., 99213 for 15 minutes, 99214 for 25 minutes) 15 minutes of 25 minute visit spent discussing goals of care/Advance Care Directives as related to their diagnosis and prognosis for CHF.
Power of Attorney for Health Care Health Care Agent/ Decision-maker Instructions For Health Care What do I want? When do I want? Why do I want?
Systematic Approach Team Roles Documentation Engagement Great Communication
Must be retrievable Supportive documentation
Game Plan Strategic plan Decide the formation -Identify patients
Have the equipment educational materials, forms Snap the ball/start the play Help initiate conversation
Timing of conversations Annual exam Initiate if involved family members present Post hospitalization When other family members/friends ill
Complete documentation Complete forms Follow up with appropriate patients Give the practice feedback
Advance Directives are stable Physicians can support the conversation CPT coding Springboard for other health plans
CaPOLST.org Caringcommunity.org Prepareforyourcare.org Go Wish cards Woodland Healthcare Advance Care Planning Discussion 530 668 2600 Ask for ACP Class under Internal Medicine