Adolescent Drug Overdose and Suicide Risks
This presentation dives into the concerning epidemiology of adolescent drug overdose and suicide, discussing various ingestions such as Skittles parties, marijuana, alcohol, and OTC medications. It sheds light on the role of social media in adolescent substance abuse and highlights risk factors, including psychosocial stresses, fixed risk factors, and mental health issues contributing to suicidal behaviors.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Drug Overdose in the Adolescent Carla Laos MD, FAAP Pediatric Emergency Medicine Physician
Objectives Provide epidemiology surrounding adolescents and overdose and suicide Discuss the medical effects of various ingestions o Skittles Parties o Marijuana, Synthetic marijuana o Alcohol o Huffing o OTC medications ( Nyquil, Listerine, Corcidin) Role of social media with adolescents and substance abuse Lack of media coverage
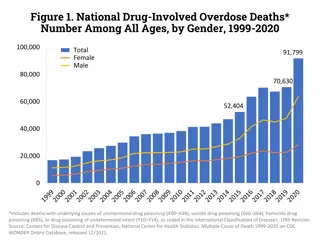
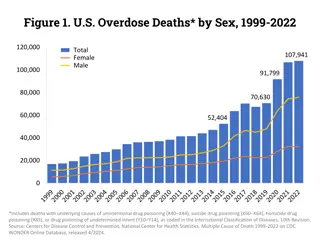
Suicide Suicide 3rdleading cause of death 15y-19y 1950-1990 suicide rate increased by 300% 1990-2013 suicide rate decreased by 20% 2013: 1748 suicides, true number may be higher Successful, Males: Females 6:1 Unsuccessful, Female: Males 2:1 National Youth Risk Behavior Survey: o 9-12 graders o 24% of students had seriously considered attempting suicide during previous year.
Fixed Risk Factors for Suicide Family history of suicide or suicide attempts History of adoption Male gender Parental mental health problems Lesbian, gay, bisexual or questioning sexual identity History of physical or sexual abuse Previous suicide attempt
Risk Factors for Suicide Psychosocial stresses o Conflicts with parents o Breakup of a relationship 15 y/o male with self inflicted wounds, large X on chest o School difficulties/failure o Social isolation (bullying) 14 year old male with Everyone hates me etched into his chest/abdomen Long term high levels of community violence may increase conduct/emotional problems and add to suicide risk for exposed youth
Mental Health Risk Factors for Suicide Sleep disturbances Depression, bipolar Substance intoxication and substance use disorders o Alcohol use/alcoholism (a/w 50% of suicides) o 15 year old dropped off by friends at DCMC, unconscious for unknown period of time. DOA. PTSD, Panic attacks, psychosis History of aggression, impulsivity, severe anger Pathologic internet use More than 90% of adolescent suicide victims met criteria for a psychiatric order before their death
Social and Environmental Risk Factors Bullying Impaired parent-child relationship Living outside the home (homeless, corrections facility, group home) School difficulties Not working or attending school Legal or romantic difficulties
Nonsuicidal Self-injury (NSSI) By definition, does not included intent to die NSSI is a risk factor for suicide attempts and suicidal ideation (Include pics)
Bullying Aggressive or deliberately harmful behavior that is: o Between peers o Repeated over time o Involves an imbalance of power (physical strength or popularity) 4 categories: o Direct-physical (assault, theft) o Direct verbal (threats, insults, name calling) o Indirect relational (social exclusion, rumors) o Cyberbullying 16 year old female ingestion of Tylenol due to spreading of naked pics on social media
Bullying Clear relationship between bullying and suicidal ideation in children and adolescents Bullying predicts future mental health problems
Internet Use Pathologic internet use correlates with SI and NSSI Video games & intenet > 5 hours a/w depression and SI/SA Suicide related seraches a/w completed suicides among young adults Participation in online forums can be dangerous o Attempts made by susceptible individuals encouraged by conversations
Leading Methods of Suicide (15-19y) Suffocation (42%) Discharge of firearms (42%) Poisoning (6%) Falling (3%)
Alcohol Most widely used psychoactive drug in the USA. Financial cost to society is $166.5 billion/year (medical treatment, rehabilitation therapy, lost earnings, car crashes) Societal double standard: o Parents will say, My kid may be drinking, but at least he s not doing drugs.
Alcohol & Teens An adolescent may employ similar logic to gain permission to drink alcohol. C mon, Dad, the three of us are just gonna split a six-pack while watching the playoffs at Andy s house. How come you and your friends get to do it and we can t? Besides, it s not like I m smoking weed or shooting up heroin. It s just beer. Address the glaring contradictions in our society. Candor will be appreciated. Here is an example of what you might say:
Alcohol and Teens It does seem hypocritical... we say it s okay for adults to drink but not to smoke marijuana. Maybe nobody should use alcohol at all, but it s such a part of our culture that I don t see us going back to the days of Prohibition. Until you turn twenty-one, you are not to drink, if for no other reason than it is against the law. Once you re of legal age, then it will be your decision whether or not to use alcohol. Illicit drugs, you are never to take; I don t care how old you are.
Alcohol & the Teenage Brain Short Term Effects: Difficulty making good decisions Less aware that behavior inappropriate or risky More likely to engage in risky behavior Less likely to recognize potential behavior Long Term Effects: Alcohol during teen years can interfere with development and change the brain Negative effects on information processing/learning Increases risk of alcohol use disorder later in life
Alcohol & Teens Additional Long-Term Effects o Blackouts, memory loss o Vitamin deficiencies o Malnutrition o Suppression of immune system o Hormonal deficiencies, sexual dysfunction, infertility o Inflammation of the pancreas (pancreatitis) o Alcoholic hepatitis o Alcoholic cirrhosis o Cardiovascular disease and stroke
Alcohol & Teens Alcohol-withdrawal delirium, or delirium tremens: o Can range in intensity from mild irritability and sleeplessness, to frightening hallucinations and delusions
Alcohol & Teens Statistics from the National Council on Alcoholism and Drug Dependence: o Alcohol use invovled in about half of all sexual assaults involving adolescents and college students, including date rape. o One in six teens admit to having experienced alcohol- induced blackouts, where they could not recall the events of the previous evening.
Alcohol & Teens Sexually active teens who overindulge are less likely to protect themselves against pregnancy and sexually transmitted diseases. Stated simply, they are too besotted to take the necessary precautions before having intercourse. The fact that heavy drinking wears down the immune system adds to their risk of contracting a sexually transmitted disease (STD).
Huffing/Sniffing According to national surveys, inhaling dangerous products is becoming one of the most widespread problems in the country. Household products such as gasoline are readily available, Has resulted in a significant rise in the number teens and young adults abusing this substance.
Huffing/Sniffing Long-Term Health Risks: Mental deterioration, chronic injury to the nervous system are the principal health dangers of chronic abuse of solvents, including gasoline. This leads to other health issues, such as: o Problems with attention, memory, and problem-solving o Muscle weakness o Tremor o Balance problems o Mood changes o Dementia o Nephritis and tubular necrosis o Certain cancers
Inhalants Inhalants Young people today can face strong peer pressure to try drugs, including a group of substances called inhalants. Inhalant abuse is particularly a problem with younger teens, but even children as young as 5 or 6 years may try inhalants. Inhalants have the special risk of being deadly any time they are used even the first time.
Inhalants Types of inhalants More than 1,000 products typically found around the house can be misused as inhalants to get high. Because these products are commonly found in homes, offices, and classrooms, they are legal, cheap, easy to get, and easy to hide. Nearly 1 in 10 eighth graders have tried inhalants. There are 3 general types of inhalants: solvents and fuels, nitrous oxide, and volatile nitrites.
Inhalants Solvents are household or industrial products that contain liquid or aerosol, including glues and adhesives, Nearly all products in pressurized spray cans can be abused, including hair spray, deodorants, computer cleaners, and spray paint. Fuels inhaled for abuse: butane, propane, gasoline, octane boosters, and refrigerants. Nitrous oxide or laughing gas is usually diverted from medical use or is found in whipping cream chargers (steel cylinder or cartridge filled with nitrous oxide used with whipping cream dispenser). Volatile nitrites found in air fresheners are mostly tried by older teens who believe this drug will enhance sexual function.
Inhalants How inhalants are used Abuse called solvent abuse, huffing, sniffing, glue sniffing, or volatile substance abuse. Users will o Sniff, huff (breathe in fumes from a rag soaked with chemicals), or inhale directly from product cans or other containers that hold inhalants. o Spray inhalants into a bag or an empty container like a soda can and inhale them. o Medical gases like nitrous oxide are often put into balloons. o Spray or pour inhalants onto a cloth or piece of clothing, then inhale deeply from the fabric.
Inhalants How inhalant use affects health Contain chemicals never meant for people to inhale. Even the first use can result in death. Heart is sensitive to inhalant effects, leading to abnormal heart rhythms and sudden death. Can cause permanent brain damage. High happens fast, lasts few seconds to minutes, unless the user inhales repeatedly. At first, inhalant users feel stimulated, but very soon feel dizzy and may slur their speech/ stumble. Sometimes users think they see things that are not there.
Inhalants Short-term effects include Excitement, no inhibition, impulsive behavior Double vision, dizziness, unsteady walking Sneezing, coughing, runny nose, red eyes Slurred speech, nausea, vomiting Sleepiness, headache, passing out Death
Inhalants Long-term effects from brain and nerve damage include Trouble with attention, poor problem-solving Muscle weakness and tremor Balance problems Poor memory, mood changes, dementia
Marijuana Marijuana use affects health and well-being School Marijuana users have a hard time thinking clearly, concentrating, remembering things, and solving problems. Frequent marijuana use often causes grades to drop. Users often lose interest in school and may quit.
Marijuana Driving and physical activity Marijuana impairs judgment, complex motor skills, and the ability to judge speed and time. Those who drive or take other risks after smoking marijuana are much more likely to be injured or killed. Sexual health Teens who smoke marijuana are more likely to take sexual risks and have unwanted or unprotected sex.
Marijuana Long-term health Teens' bodies and brains are still growing and maturing, so smoking anything, including marijuana, is not good for lung health. Marijuana use may also lead to addiction or mental health problems (ie, depression, anxiety or schizophrenia).
Cough & Cold Medicines Dexamethorphan acts onsame receptors as ketamine or PCP Causes hallucinations Codeine binds to same receptors as heroin Both codeine and DXM increase dopamine in the brain s reward pathway
Cough and Cold Medicines Abuse of DXM can cause: o Loss of coordination o Paresthesias o Nausea o Elevated BP, HR o Rarely, hypoxia, causing brain damage when DXM taken with decongestants Abuse of Promethazine- Codeine Cough syrup o Bradycardia o Slowed breathing ( high doses can lead to overdose and death) These medications even more dangerous when taken with other drugs
Protective Factors Religious involvement Connection between teen and parents, school and peers
Approaching the Adolescent No data indicate that inquiry about suicide precipitates the behavior. Suicidal thoughts or comments should never be dismissed. Behavioral problems that may be manifestations of masked depression o Truancy o Academic deterioration o Running away o Defiance of authorities o Drug/Alcohol abuse o Delinquency o Sexual acting out
Approaching the Adolescent Screen patients for suicide, mood disorders and substance abuse/dependence Ask about emotional difficulties, use of drugs/alcohol Assess level of danger to self/others Where resources lacking, others encouraged to obtain extra training and become competent in providing an in depth assessment
Role of Media Youth may imitate suicidal behavior seen on television Media coverage of an adolescent s suicide may lead to cluster suicides o Additional deaths directly proportional to amount/duration/prominence of media coverage
Management of the Suicidal Adolescent Management depends on risk Adolescents at high risk: o Plan or recent suicide attempt o Stated current intent to kill themselves o Recent SI or behavior accompanied by current agitation/hopelessness o Impulsivity and profoundly dysphoric mood a/w bipolar, depression, psychosis or a substance abuse disorder Those who seem at low risk, joke, or seek help for repeated somatic complaints may be asking for help.
Management of the Suicidal Adolescent Moderate or high risk of suicide or attempt: o Immediate mental health professional evaluation o Options include hospitalization, transfer to emergency department, same day evaluation by MH professional Consider psychiatric hospitalization o Previous attempts o High degree of intent to commit suicide o Serious depression or other psychiatric illness o Engage in substance abuse/have active substance use disorder o Low impulse control o Families unwilling to commit to counseling
Careful of the Suicide Gesture This term should not be used. Adolescent who took 8 Motrin tablets: o May have thought it was lethal and may do something more lethal the next time o May hae known dose was not lethal and took the pills as a rehearsal for a lethal attempt The benefit of the doubt is generally on safety in the management of the suicidal adolescent
References Suicide and Suicide Attempts in Adolescents, Committee on Adolescents. Pediatrics Apr 2000, 105 (4) 871-874; DOI Suicide and Suicide Attempts in Adolescents Committee on Adolescence. Pediatrics Jul 2016, 138 (1) e20161420; DOI: 10.1542/peds.2016-14204 National Institute of Mental Health (best practices for media and online reporting of deaths by suicide) Teens.drugabuse.gov National Institute on Drug Abuse (NIDA) drugabuse.gov