Addressing Insurance Barriers in Eating Disorder Treatment: A Call for Change
Kentucky faces significant challenges in providing adequate care for individuals with eating disorders due to insurance barriers, lack of trained professionals, and limited treatment options within the state. The high mortality rate, chronic nature, and costly treatment of eating disorders exacerbate the situation. Efforts are needed to improve access to quality care, training for providers, and support systems for affected families to address the urgent need for better mental health parity and treatment options.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Mental Health Parity & Eating Disorder Treatment Insurance Barriers November 9, 2021 Presented by: Melissa Cahill (Kentucky Eating Disorder Council; Chair) Justin Wallen (Louisville Center for Eating Disorders; Business Manager) Dr. Andrea Krause, MD (Norton Children's Hospital) Ruby Jo Lubarsky (Kentucky Resident)
Eating Disorders Are an Epidemic In Kentucky there are roughly 900,000 individuals with an eating disorder Of these 900,000 there are 29,804 children with this life-threatening condition There are ZERO acute care programs, residential programs or partial hospitalization programs in Kentucky Kentucky residents are forced to go out of state to receive needed care above the outpatient level Individuals with Medicaid have few or no options for higher levels of care out state.
Burden of Eating Disorders High morality rate Anorexia nervosa has the second highest mortality rate of ANY psychiatric illness Debilitating Average time from diagnosis is 10 years Often becomes chronic illness Costly Treatment costs on average $20,000 per month Not accounting for lost time at work, school, etc.
Determine best practice diagnostic treatment, prevention, early intervention, and recovery services Evaluate support systems for families and promote the acquisition of quality care and training for providers Identify the magnitude of the problem and treatment needs for Kentucky citizens MORE AVAILABLE, ACCESSIBLE, AND AFFORDABLE CARE FOR KENTUCKY RESIDENTS MAJOR ROADBLOCK-CURRENT MENTAL HEALTH INSURANCE PRACTICES IN KENTUCKY
LACK OF PROVIDER PARTICIPATION WITH INSURANCE PLANS Insurance Barriers for Eating Disorder Treatment LIMITED NUMBER OF TRAINED EATING DISORDER PROFESSIONALS IN KENTUCKY REVIEW CRITERIA FOR EATING DISORDER TREATMENT DOES NOT TAKE INTO ACCOUNT THE COMPLEX NATURE OF THIS ILLNESS ADDITIONAL COST FOR IN NETWORK OUT OF STATE TREATMENT Travel cost, lodging, provider fees, medication, and labs INDIVIDUALS THAT ARE ABLE TO FIND CARE OUT OF STATE ARE LEFT WITH NO OPTIONS FOR STEP DOWN CARE WHEN THEY RETURN HOME THE CYCLE CONTINUES
LACK OF PROVIDER PARTICIPATION WITH INSURANCE PLANS A 2017 report by Milliman confirmed that reimbursement rates for mental health and substance use disorder treatment providers, through private insurance plans, were far lower than reimbursement rates for other medical providers, relative to Medicare rates. When insurance plans do not reimburse providers adequately, many choose not to participate in the plans networks. So, when someone makes a decision to seek help yet they are unable to find a provider in network they often have to go out-of-network, resulting in higher costs. Many people give up simply because they can t afford treatment
2015 Inpatient out of network use 4.2x higher for mental health Network Utilization Rates for PPO Plans by Care Setting 2015 Outpatient out of network use 5.8x higher for mental health (compared to primary care) 2015 Office visits out of network use 5.0x higher for mental health
In-Network Provider Payment Levels Relative to Medicare Kentucky All office visits Year Primary care Behavioral Health Reimbursement Differential 2013 102% 75% 35.1% 2014 101.1% 82.4% 22.7% 2015 93.7% 71.8% 30.4%
Additional Problems LIMITED NUMBER OF PROVIDERS IN THE STATE TRAINED IN EATING DISORDER TREATMENT The American Academy of Pediatrics last year estimated the need for child psychiatrists at 47 per 100,000 people, roughly four times the number in practice. (wsj 6/27/21 Americans Seek Urgent Mental Health Support as Covid 19 crisis ebbs) INSURANCE REIMBURSEMENT RATES PROVIDE NO INCENTIVE FOR PROVIDERS TO TREAT EATING DISORDERS OR ATTRACT TRAINED PROFESSIONALS TO OUR STATE COMPLEX DISORDER REQUIRE TEAM APPROACH Insurance companies don t compensate for coordination of care of multidisciplinary teams
Additional Problems MANY ARE GEOGRAPHICALLY UNABLE TO ACCESS CARE TELEHEALTH SUPPORT SHOULD PERSIST AFTER THE COVID 19 PANDEMIC Easing of licensure laws to allow cross-state practice would ensure individuals with anorexia nervosa who come from states and regions that lack specialty care can still access evidence-based interventions. - Bulik AJP PROVIDERS THAT DO TREAT EATING DISORDERS ARE OVERWHELMED BY DEMAND AND OFTEN DON T HAVE OPENINGS
Interference of Managed Care in Course of Treatment Hospital discharge decisions should not only consider weight gain, but also cognitive, affective, and behavioral aspects of the illness, and care should be taken to ensure a seamless transition to lower levels of care. (Bulik, 2021) Due to strict and narrow review criteria PATIENTS ARE OFTEN DISCHARGED PREMATURELY FROM TREATMENT THIS CREATES A MUCH HIGHER RELAPSE RATE Having a full-time employee in a treatment center whose main responsibility is to perform utilization reviewswith insurance companies demonstrates just how much time is spent having to advocate for sufficient treatment. & PREVENTS CONTINUITY IN TREATMENT FOR THE INDIVIDUAL The reviewer .often has no clinical experience in the disorder which the client suffers. Elyse Rochman, LCSW
Only Higher level of care in KY offering Evidence-Based Treatment for Eating Disorders Highly Educated Professionals Doctoral and Masters level with specialty training in eating disorders Requires adequate compensation to sustainably perform this work and continuing education Timeline of Insurance Involvement Intensive Outpatient Started ED IOP in Oct. 2017 (out-of-pocket) First In-Network early 2019 Seeking re-negotiation (since January 2021) Partial Hospitalization Requires insurance contracts Ready to start program and began application process January 2021 Difficult Process Insufficient rates to adequately sustain or grow the business
Experience Being In-Network with Insurance for Eating Disorders Business Full-time staff devoted to handling insurance issues (cost, frustration) Significant therapist involvement (less time for patient care) to complete Doc to Doc reviews due to insurance not thinking patient is sick enough to be in care longer. Last-minute denials ? LCED providing unreimbursed care because inappropriate to abruptly end treatment for a life-threatening problem. Patients Utilization Reviews/Cutting Off Treatment Arbitrary decisions by individuals with no ED experience State Indicative of systemic problems for the treatment of mental health
Dr. Andrea Krause, MD Norton Children s Hospital
Dr. Andrea Krause, MD The inpatient acute medical stabilization is the catch all I see the failures of the system as a whole Poor recognition due to inadequate provider training leads to delayed outpatient care Poor access and number of providers needed to see these patients lead to further delay in treatment While this delay occurs, the patients simply downward spiral Ultimately, they become near death, and need hospitalization.
Dr. Andrea Krause, MD 2021 has seen an almost 2-fold increase in number of hospitalized patients for eating disorders. This is on top of a year-to-year 20 percent increase in the past 10 years. They are sicker than ever, and I believe this is due to lack of access to care in the outpatient setting Payor mix breakdown in years past was 60 percent private insurance, 40 percent Medicaid. This trend continues MEDICAID PATIENTS CURRENTLY HAVE 1 OPTION IN STATE AND THAT IS OUTPATIENT/IOP (LCED) Insurance payors do not seem to be aware of published guidelines on Levels of Care for Eating disorders (APA, AAP) When kids are hospitalized for eating disorders, they generally fulfill criteria for needing residential treatment: this means seeking care out of state
Dr. Andrea Krause, MD Currently no out of state residential facility has an active Kentucky Medicaid number. There are a few that have recently expired. Due to poor reimbursements, I suspect these facilities have little to no incentive to renew their KY Medicaid numbers. Due to this: Medicaid patients stay for MONTHS in the hospital due to lack of placement options. This is detrimental to getting adequate treatment for their disorder.
Ruby Jo Lubarsky will give her first-hand experience regarding the challenges of eating disorder treatment access.
KENTUCKY MUST CHANGE ITS MENTAL HEALTH INSURANCE LAWS IMPROVE REIMBURSEMENT RATES TO EXISTING MENTAL HEALTH PROVIDERS SO THAT THEY CAN PARTICIPATE WITH INSURERS SO THAT MORE KENTUCKIANS CAN RECEIVE CARE IMPROVE CREATE INCENTIVES FOR PRACTITIONERS TO WANT TO PRACTICE IN KENTUCKY BETTER REIMBURSEMENT RATES, TAX INCENTIVES, EDUCATIONAL OPPORTUNITIES CREATE CHANGE THE REVIEW CRITERIA FOR EATING DISORDER CARE TO ACCURATELY REFLECT THE TREATMENT NEEDS OF THIS COMPLEX, LONG TERM, SERIOUS ILLNESS CHANGE EASE EASE CROSS STATE LICENSING LAWS FOR TELEHEALTH EVIDENCE BASED ACCESS TO CARE
With Mental Health Insurance Reform We Can Stop This Cycle Insurance companies discharge patient to lower levels of care as quickly as possible due to high cost of treatment. greatest risk for relapse is the ~60-day period after discharge from inpatient or day treatment. - Bulik Individual must go out of state for higher levels of care Out of Network Care no participating provider The burden that our broken system puts on patients and families is incalculable emotionally, and financially amounts to ~64.7 billion annually, equating to $11,808 per person with a eating disorder - Bulik Individual returns to Kentucky where there are no step -down programs which take insurance.
Provider Testimony with the lack of access to care and difficulty with reimbursement Lynn Supple, PsyD, HSP Aspire Wellness, Louisville KY insurance has proved to be one of the biggest obstacles in allowing people to access eating disorder care with me or within my practice. We cannot be in-network as the rates will not allow us to sustain quality work. Insurance also prevents clients from seeking care in the first place, which allows the eating disorder to get worse, and ultimately taxes insurance more (not to mention the trauma for the individual and family.) Elyse Rochman, LCSW Private Practice, Goshen KY The truth is that there was too much paperwork, too much red tape, and reimbursement rates were ridiculously low. I couldn t afford to pay someone to do my insurance billing because I was barely making enough to stay afloat. Eating disorders also have the highest mortality rate of all psychiatric diagnoses, so when we are talking about appropriate levels of care, we are potentially talking about matters of life and death.
Provider Testimony with the lack of access to care and difficulty with reimbursement Jennifer Kendrick, LCSW--True North Counseling, Louisville KY The first thing that comes to mind is the difficulty that I have had getting clients to higher levels of care. Life-saving help should not be dependent on the type of insurance a person has, but it is the reality here in Kentucky. I have had to send clients as far as California and Colorado so that they can get the care that they need, which means that they are separated from their families during an incredibly stressful time for the whole family unit. Families should not have to choose between supporting one another and life and death.
Provider Testimony with the lack of access to care and difficulty with reimbursement Tina Thompson, RD - Bluegrass Nutrition Counseling, Lexington KY As a registered dietitian who specializes in eating disorders, insurance coverage for my clients is essential. There is little to no hesitation about scheduling an appointment and moving forward in recovery. They are seen regularly without the financial burden associated with a possibly lengthy recovery time. If insurance does not cover, they may receive counseling from others with little to no experience in this field or they may choose to not pursue recovery at all both creating increased economic costs and reduced wellbeing of the client.
Additional Testimonies Melissa Cahill Now that my daughter is newly financially independent, she has had to drop her long time out of network therapist. She cannot afford even the sliding scale amount per appointment. She has tried to make it work at a student run clinic at her University but it has proved to be difficult. She does not have a dietician again, none on insurance that treat eating Disorders. She is scrambling to find care she can afford and this is all after being discharged in July from a higher level of care.
Additional Testimonies Marilyn Clark Insurance had a time frame for you to be in and out. When Aubrey was on disability, residential programming was not covered at all, so she basically went from in patient to on the street , and maybe once a week appointments with a therapist because again, no one in our area had specialized programs-groups, support groups, trained ED therapists, and even doctors. We continued in the cycle of out-of-state ED clinics and hospitals, coming home to no support, going out of state. Aubrey passed away in 2005 from complications of her eating disorder. Could this have been prevented if she had been treated sooner ? If there was outpatient care available early on and when she was discharged from treatment?
Articles for Additional Information Americans Seek Urgent Mental-Health Support as Covid-19 Crisis Ebbs The Wall Street Journal Why It s So Hard to Find a Therapist Who Takes Insurance The Wall Street Journal From Awareness to Action: An Urgent Call to Address the Inadequacy of Treatment for Anorexia Nervosa Cynthia M. Bulik, Ph.D.
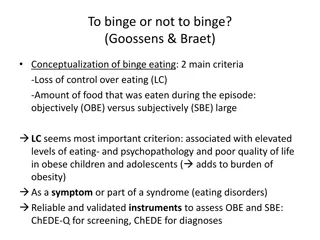
References Berends et al., 2016 Chesney et al., 2014 Fairburn et al., 1995 Fichter & Quadflieg, 2016 Hudson & Pope, 2018 Kass et al., 2013 Khalsa et al., 2017 Smink et al., 2012 Suokas et al., 2013 Deloitte Access Economics, 2019
Thank you! If you have any questions regarding this presentation or would like to contact one of the presenters, please email or call. Melissa Cahill, Chair Kentucky Eating Disorder Council melliottcahill@gmail.com 502-594-4279