ABSENCE SEIZURES
Absence seizures usually start at 5-8 years of age, often overlooked due to their brevity. Typical characteristics include brief consciousness arrest, eye flutter, and immediate resumption of activities. Unlike complex partial seizures, absence seizures lack aura and typically last only a few seconds. Hyperventilation can trigger these seizures, prompting a 3 Hz spike-and-slow-wave discharge. Most children outgrow absence seizures, but some may develop generalized tonic-clonic seizures. Infantile spasms, a rare seizure disorder in young children, present with flexor, extensor, or mixed muscle contractions. Early diagnosis and appropriate treatment are crucial for managing these conditions effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
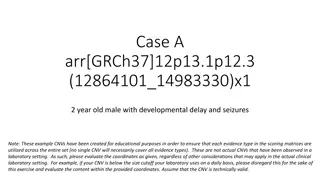
Typical absence seizures usually start at 5-8 yr of age and are often, owing to their brevity, overlooked by parents for many months even though they can occur up to hundreds of times per day
The characteristic of the attack is a brief arrest of consciousness usually for 5-10 sec. appearing without warning or aura. There can be a slight loss of tone causing the child to drop objects from his hands but it rarely enough to induce a fall.
Unlike complex partial seizures they do not have an aura, usually last for only a few seconds, and are accompanied by eye lid flutter or upward rolling of the eyes but typically not by the usually more florid automatisms of complex partial seizures (starring, chewing, wandering, confused speech). Absence seizures do not have a postictal period and are characterized by immediate resumption of what the patient was doing before the seizure.
Hyperventilation for 3-5 min can precipitate the seizures and the accompanying 3 Hz spike and slow-wave discharge.
Most patient outgrow seizures before adulthood , but 25% develop generalized tonic-clonic seizures. Treatment Eth0suximide 20 mg/kg sodium valproate Clonazepam
Infantile spasm West syndrome Salam's attack
Infantile spasms (IS) is a rare seizure disorder that occurs in young children, usually under one year of age. The average age of onset is around four months. A few children may begin as late as two years. Spasms can be flexor, extensor, or a mixture of flexion and extension. Flexor spasms consist of brief contractions of the flexor muscles of the neck, trunks, and limbs, resulting in a brief jerk.
Extensor spasms consist of contractions of the extensor musculature, with sudden extension of the neck and trunk and with extension and abduction of the limbs. Mixed spasms are the most common type These attacks occur in clusters throughout the day and last anywhere from less than 1 minute to 10-15 minutes or longer in some patients. Spasms frequently occur just before sleep or upon awakening.
Etiology One theory states that the effect of different stressors in the immature brain produces an abnormal, excessive secretion of corticotropin- releasing hormone (CRH), causing spasms.The clinical response to adrenocorticotropic hormone (ACTH) and glucocorticoids can be explained by the suppression of CRH production.
Infantile spasms can be classified according to their suspected etiology as symptomatic, cryptogenic, or idiopathic. Symptomatic Patients are diagnosed with symptomatic infantile spasms if an identifiable factor is responsible for the syndrome. Virtually any disorder that can produce brain damage can be associated with infantile spasms. The list of etiologies can be subdivided into prenatal disorders, perinatal disorders, and postnatal disorders. Tuberous sclerosis Hypoxic-ischemic encephalopathies Congenital infections Trauma Meningitis Encephalitis Inborn error of meabolism
-Cryptogenic Patients have cryptogenic infantile spasms if no cause is identified, but neurologically abnormal. . -Idiopathic Patients may be considered to have idiopathic infantile spasms if normal psychomotor development occurs prior to the onset of symptoms, no underlying disorders or definite presumptive causes are present, and no neurologic or neuroradiologic abnormalities exist.
Interictal electroencephalogram Hypsarrhythmia (seen in the image below) is the characteristic interictal EEG pattern. It consists of chaotic, high- to extremely high voltage, polymorphic delta and theta rhythms with superimposed multifocal spikes and wave discharges.
Medications such as ACTH, vigabatrin (may cause visual field defect) , and conventional antiepileptic drugs (AEDs) are the mainstay of therapy for infants with West syndrome. Unfortunately, no single medical treatment gives satisfactory relief for all infants with West syndrome. ACTH 20 unit/kg IM for 2 weeks followed by 40 unit/kg for 4 weeks