Comprehensive Management Guidelines for Pediatric Eating Disorders
This comprehensive guide covers the management of children and young persons with eating disorders, focusing on anxiety, confusion, knowledge, and skill development. It emphasizes the partnership between pediatricians and psychiatrists, specific medical and nutritional aspects, adequate support, and advice for medical care and psychiatric treatments. The document explores risk assessment, physical examination, location of care, transition between services, compulsory treatment, re-feeding, managing compensatory behaviors, discharge planning, and more. It also provides practical recommendations for medical staff, nursing support, family involvement, and multidisciplinary teamwork in treating pediatric eating disorders.
- Pediatric Eating Disorders
- Medical Management
- Psychiatry Partnership
- Nutritional Aspects
- Compulsory Treatment
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
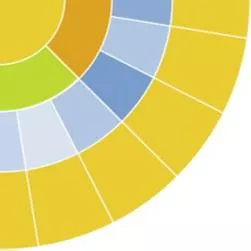
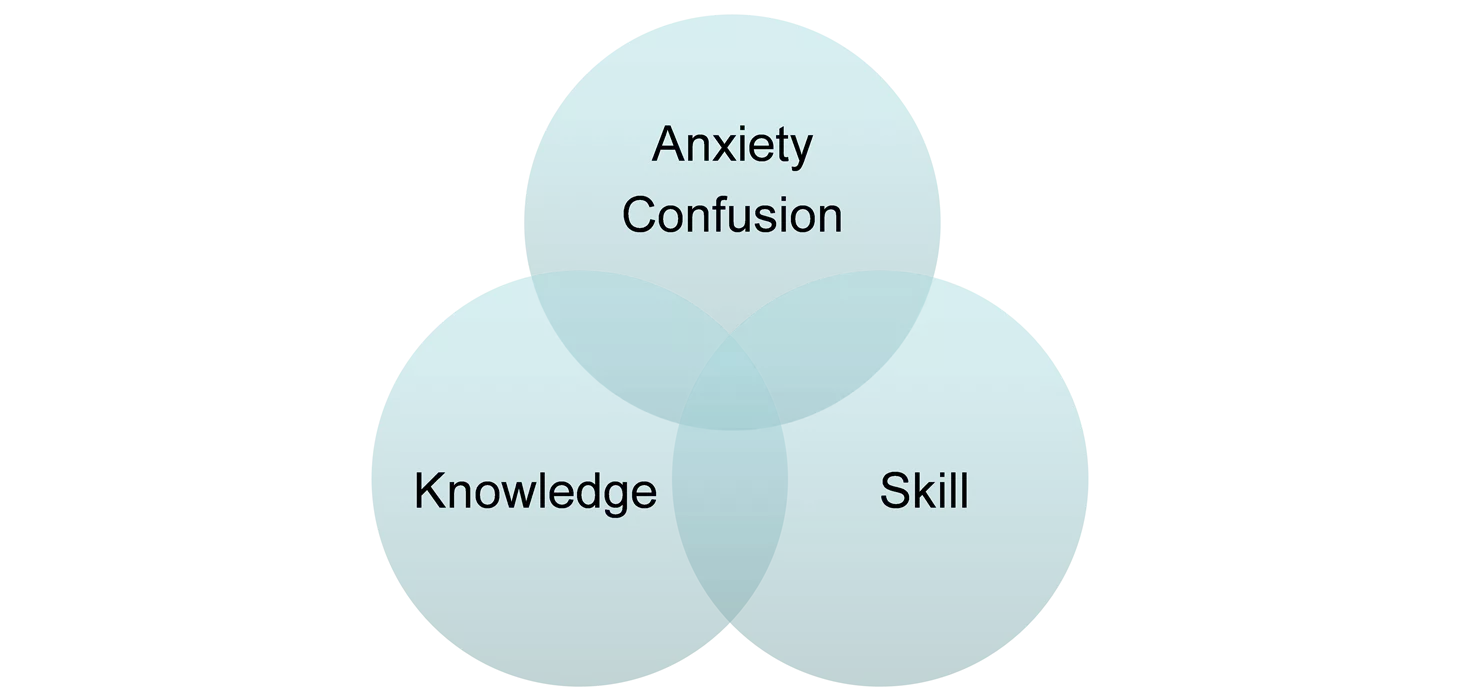
A child/young person with ED on the ward Anxiety Confusion Knowledge Skill
A partnership between paediatrician and psychiatrist Specific medical and nutritional aspects (Paediatrician, paediatric nursing staff, dietician) Adequate support and advice to the medical care and specific psychiatric treatments (Specialist Surrey ED team)
Eating Disorders in Children and Adolescents Management of the Really Sick Patient with Anorexia nervosa (MARSIPAN)
Guidance from the Junior MARSIPAN Risk assessment, physical examination and associated action Location of care and transition between services Compulsory treatment Paediatric admission and local protocols Management of re-feeding Management of compensatory behaviours associated with an ED in a paediatric setting Management in primary care and paediatric out patient settings Discharge from paediatric settings Management in specialist CAMHS in-patient settings
Recommended Practice Guidelines on medical management aimed primarily at junior staff A guide for nursing and medical staff on supporting parents and families Regular staff meetings to ensure a consistent approach and minimise the risk of splitting Regular multidisciplinary team meeting weekly or more Review progress, review future plans and record and discharge planning Formulate a nursing plan
Overview Medical Reasons for a paediatric admission Presentations Behavioural Manifestations Families Risk Assessment Key assessment parameters and action points Compulsory Treatment Some practical considerations and dietetic input Re-feeding Syndrome Discussion of a case
Medical reasons for in-patient paediatric admission The need for IV fluids to correct electrolyte abnormality Re-feeding for severe malnutrition Management of physical complications of severe malnutrition and/or associated behaviours (eg Purging) Management of acute medical illness unrelated to anorexia nervosa if present
Presentations Anorexia nervosa Refusal to maintain body weight or failure to gain weight during a period of growth Intense fear of gaining weight Disturbed body perception Undue influence of body weight or shape on self-esteem Denial of seriousness of current low body weight Secondary amenorrhoea in girls post-menarche.
Behavioural Manifestations Excessive exercise/Activity Purging Bingeing Self-harm Co-morbid psychiatric conditions OCD, Anxiety, Depression Violent and disturbed behaviours
Families Families do not cause eating disorders Parents are the best considered partners in recovery Families are organised by the eating disorder Parental anxiety can be high Separation anxiety is common NICE guidelines
Risk Assessment Medically compromised children can be very unwell and can die of complications Complexities of managing are compounded by the anxieties of the parents and their family (this can impact caring teams) It is easy to feel de- skilled Risk assessment includes: Clinical assessment with investigations Assessment of motivation and engagement with treatment plans Available parent/carer support
Risk Assessment Framework (1) BMI and weight <70% (approx <0.4thBMI centile) Recent loss of weight of 1Kg or more/week for 2 consecutive weeks % median BMI % median BMI 70-80% (approx 2nd-0.4thBMI centile) Recent loss of weight 500- 999g/week for 2 consecutive weeks % median BMI 80-85% (approx 9th-2ndBMI centile) Recent weight loss of up to 500g/week for 2 consecutive weeks % median BMI > 85% (approx >9thBMI centile) No weight loss over past 2 weeks CVS Health HR <40bpm (awake) HR 40-50 bpm (awake) Sitting BP systolic < 0.4th centile (84- 98mmHg); diastolic <0.4th centile (35- 40mmHg) HR 50-60 bpm (awake) Sitting BP systolic <2nd centile (98- 105mmHg); diastolic (0.2nd centile (40- 45mmHg) HR >60 bpm (awake)
Risk Assessment Framework (2) H/o recurrent syncope; marked orthostatic changes (fall in systolic pr 20mmHg or more or increase in HR of >30bpm) Irregular heart rhythm QTc>460ms (girls) or 400ms (boys) with brady/tachyarrh ythmia Occasional syncope; moderate orthostatic changes (fall in systolic pr 15mmHg or more or increase in HR of up to 30bpm) Pre-syncopal symptoms but normal orthostatic CVS changes Normal orthostatic CVS changes Cool peripheries Normal hearth rhythm QTc <460ms (girls) or 400ms (boys) ECG abnormalities QTc >460ms (girls) or 400ms (boys) QTC <460ms (girls) or 400ms (boys) Medication/fami ly history
Risk Management Framework (3) Hydration status Fluid refusal Severe dehydartion (10%) Severe fluid restriction Moderate dehydration (5- 10%) <36 C Fluid restriction Mild dehydration (<5%) Not clinically dehydrated Temperature <35.5 C tympanic or 35 C axillary Hypophosphata emia, hypolalaemia, hypoalbuminae mia, hypoglycaemia, hyponatremia, hypocalcaemia Biochemical abnormalities Hypophoaphata emia, hypokalaemia, hyponatraemia, hypocalcaemia
Risk Management Framework (4) Disordered eating behaviours Acute food refusal or estimated calorie intake 400-600 kcal/day Severe restriction (, 50% of required intake), vomiting, purging with laxatives Poor insight into eating problems, lacks motivation to tackle eating problems, Moderate restriction, bingeing Engagement with management plan Violent when parents try to limit behaviour or encourage food/fluid intake, Some insight into eating problems, some motivation to tackle eating problems, Some insight into eating problems, motivated to tackle eating problems,
violence in relation to feeding (hitting before feeding) resistance to changes required to gain weight, parents unable to implement meal plan advice given Moderate levels of uncontrolled exercise in the context of malnutrition (>1h/day) ambivalent towards changes required to gain weight but not actively resisting ambivalence towards changes required to gain weight not apparent in behaviour Activity and Exercise High levels of uncontrolled exercise in the context of malnutrition (>2h/day) Mild levels of uncontrolled exercise in the context of malnutrition (<1h/day) No uncontrolled exercise
Key physical assessment parameters and action points Check for/measure What to look for When to be concerned (Amber/red) <50bpm or symptomatic postural tachcardia Prolonged QTc, HR<50, arrhythmia associated with malnutrition and/or electrolyte disturbance Systolic, diastolic or mean arterial pr < 0.4thcentile and/or postural drop > 15mmHg Specific management Heart rate Bradycardia, postural tachycardia Nutrition, ECG ECG Other cause for bradycardia, arrhythmia, check QTc time and electrolytes Nutrition and correct electrolyte abnormalities, increased QTc-bed rest, discuss with cardiologist Nutrition, bed rest Blood pressure Hypotension- refer to statndardised charts for age and gender
Key physical assessment parameters and action points (2) Check for/measure What to look for When to be concerned (Amber/red) Specific management Hypothermia Temp <36 C will usually be accompanied by other features. Beware of <35 C Nutrition and blankets Dehydration Hypotension and bradycardia usually related to malnutrition Significant degydration ORS orally or via NG tube preferred unless hypovolaemia; check electrolytes and renal function
Key physical assessment parameters and action points (3) Check for/measure What to look for When to be concerned (Amber/red) Specific management Hypovolaemia Tachycardia or inappropriate normal HR in undernourished pt, hypotension and prolonged capillary refill time Lanugo hair, dry skin, skin breakdown and/or pressure sores Senior paediatric review. Normal saline 10ml/kg bolus then review. Add electrolytes as required eg phosphates Nutrition; seek specialist advice for skin breakdown or pressure sores Other features of severe malnutrition
Key assessment parameters and action points (4) Check for/measure What to look for When to be concerned (Amber/red) Specific management Evidence of purging Low K, metabolic acidosis or alkalosis, enamel erosion, swollen parotid glands, calluses on fingers Likely to be due to purging Hypokalaemia, uncontrolled vomiting with risk of oesophageal and other visceral tears Specialist nursing supervision to prevent vomiting Hypokalaemia <3mmol/l admit; consider HDU, PICU, ICU if <2- 2.5mmol/l <130mmol/l admit: consider HDU etc if <120-125mmol/l Correction IV initially if <3mmol/l ECG Hyponatraemia or hypernatraemia Consider water loading If IV correction proceed with care
Key assessment parameters and action points (5) Check for/measure What to look for When to be concerned (Amber/red) Specific management Other Electrolyte abnormalities Check PO4 magnesium and calcium Hypoglycaemia Relatively rare and implies poor compensation or coexisting illness- admit Psychosocial assessment as per NICE guidance Oral or NG correction where possible; IV bolus if severe Mental health risk/safeguarding/ family Suicidality, self harm, family not coping CAMHS involvement. Apply local safeguarding procedures as needed
Compulsory Treatment Mental Health Law Young people <16 can be treated against their will if at least one parent consents to treatment on their behalf. If the child actively fights the parent s decision compulsory treatment needs to be considered 16-18 year olds can be admitted under the MHA and treated against their will If both child and parent refuse treatment, local safeguarding procedures should be followed and use of the Children Act might be necessary (up to the age of 18)
Other compulsory treatments for <18 Children Act 1989 Specific issue Order (section 8) can be used to pass a NG tube Care Order (section 37) can be applied if a child is thought to be at risk of significant harm because of care given or not given Inherent Jurisdiction of the Court (section 100) can be used to treat against a child s will when there are wider-ranging and longer-term issues UN Convention on the Rights of Children 1991 Children s right to form and express their views (Article 12) Best interests of the child (Article 3) Responsibilities, rights and duties of parents (Article 5)
Some practical considerations Place of nursing general not separate cubicle Nursing care Identify core group of nurses to provide continuity and consistency Special nursing- appropriate training Parent s role Education Teaching staff need to be aware Social interaction Time off ward May require restriction
Dietetic Input Paediatric dieticians are essential Devise a safe meal plan and agree with team and family (consult parents) Meal plan should ideally comprise solid food. Make up with Fortisip if meal is not completed If unable to meet the presribed calorie intake within 24 hours consider insertion of NG tube (balance the risk and wishes of child/parents) In early stages of re-feeding meal plans should not exceed the recommended guidelines of 50% TEI
Re-Feeding Syndrome Sudden reversal of prolonged starvation Sudden requirement for electrolytes involved in metabolism Abnormal electrolytes Phosphate levels fall very rapidly within the 1stweek of re- feeding with neurological and cardiovascular consequences
Re-feeding syndrome No evidence based guidelines for re-feeding A common recommendation is to increase daily from a baseline intake by 200kcal/day If phosphate drops, intake should be static until it stabilises Blood tests done daily in the first 2-5 days and repeat after 7-10 dyas Syndrome can develop later and blood tests should continue for 2 weeks or until stable
Case Discussion 15 year old girl- Amy . Parents, 13 year old sister Monday: Private GP: wt: 32kg, Ht:161cm Marginally low PO4; murmur. ?wt 36kg x 2 years Wednesday: Sent to local DGH for inv of murmur-Found to have MR. Possibly congenital? Or effect of ED? Thursday: CYPS EDS: wt: 29kg W4H: 54% Now eating more
Case Discussion Friday: Back to DGH. Private assessment cancelled W/E: Back to DGH Monday: Assessment ED inpatient unit Tuesday: ???