Quality Improvement in Emergency Care: Challenges and Solutions
Widespread dissatisfaction with clinical audits has highlighted the need for quality improvement projects in Emergency Care, becoming a crucial skill for NHS Consultants. The Royal College of Emergency Medicine emphasizes patient-centered, timely, efficient, safe, and equitable care through evidence-based guidelines and avoiding wasteful practices. RCEM audits focus on standards - fundamental, developmental, and aspirational - ensuring minimum safety and quality levels are met. Challenges in audit improvement include turning it into a meaningful activity rather than a tick-box exercise, providing feedback loops, overcoming temporary staff limitations, and prioritizing care advancement over career advancement.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Quality Improvement Adrian Boyle Chair of the Quality Emergency Care Committee @dradrianboyle
Background Widespread dissatisfaction with clinical audit Quality Improvement Projects likely to become as part of FCEM Understanding quality improvement will be a necessary skill for NHS Consultants
Quality Safe Timely Effective Efficient Equitable People aren t discriminated against Patient Respectful Centred Patients aren t harmed Within an appropriate time frame Evidence based guidelines are Avoids waste
Timeliness Patient Centred Safety Efficient Effective Equitable The Royal College of Emergency Medicine
Patient Centred Timeliness Efficient Safety Equitable Effective The Royal College of Emergency Medicine
RCEM Audits 12th Year Process and documentation audits Common, important conditions Across the life span Not audited well elsewhere Supported by HQUIP Quality Accounts
RCEM Audits: Standards Fundamental Developmental Aspirational
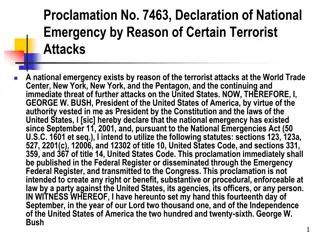
Fundamental Standards Fundamental standards of minimum safety and quality - in respect of which non-compliance should not be tolerated. Failures leading to death or serious harm should remain offences for which prosecutions can be brought against organisations.
So which of your current standards are fundamental ? All patients with a hip fracture should receive analgesia within 4 hours All patients with a hip fracture should be offered analgesia within four hours
Why does audit fail to improve care? Tick box exercise Performed by temporary staff Lack of feedback loops Career advancement rather than care advancement Lack of collective responsibility Strangled with red tape
Fractured Neck of Femur Patients Receiving Analgesia within One Hour %
Quality Assurance Quality Improvement Motivation Measuring compliance Continuously improving processes to meet standards Means Attitude Focus Scope Responsibility Inspection Defensive Outliers Medical Provider Few Prevention Chosen, proactive Processes Patient care All
The Anatomy of an Audit Structure Does your ED have a PLAN compliant room? Process Can your ED give analgesia promptly? Outcome Did a child die during a seizure in your ED?
The Anatomy of an Audit (2) Local Benchmarking National Picture Safety of sedation in UK EDs Timeliness of psychiatric assessment Aggregation of less common cases Status Epilepticus
The Future of the Audit Program Rapid cycle methodology (?2016-17) Initial performance Intervene Quick repeat of failed standards on a smaller group Increased Consultant and team ownership Endorsement by relevant bodies Public domain Narrative for adverse outcomes
Public Domain Accessible to all Easily interpretable by all
Narrative and Hard Numbers Hearts and Minds 52% of your hip fracture patients received analgesia within 60 minutes of arrival An 86 year old lady with mild dementia fell at home and broke her hip. The triage nurse recorded her pain score at 9/10. She was assessed by a junior doctor who prescribed intravenous morphine at 180 minutes after arrival. This wasn t administered until after arrival on the ward six hours after her fall.
Improvement Science Industry developed Limited evidence of effectiveness in healthcare
Quality Improvement Approaches (1) Business Process Re-engineering Fundamental rethinking of process from the centre Visionary Leader Experience based co-design Ask patients and staff to identify touch points (the bits that matter)
Quality Improvement Approaches (2) Lean (Toyota) Regulating flow Reducing waste Pull mechanisms to support flow Model for Improvement PDSA Six Sigma Customer defined defects
Quality Improvement Approaches (3) Statistical process control Control charts for acceptable versus unacceptable variation Theory of constraints Identify bottlenecks and targeting resource Total Quality Management Philosophy
Basic Principles of all methods Measurement for improvement Hypothesis can change throughout the project Data has to be good enough , not perfect Process Mapping Improving reliability Demand, capacity and flow Empowering staff
Waiting room Minors nurse Discharge ENP Receptionist Secondary Assessment by Minors nurse, pick up card from box Minors nurse SpR/ In Patient Pharmacy Presenting complaint Treatments Patient registered by receptionist at reception. Card then placed by patient in box next to minors Consultant Analgesia / ECG / Sometimes x-ray / sometimes Liaise PA Medical Assessment Minors Minors nurse Patient arrives at the ED on foot Initial Assessment by pre-reg nurse Infection Control Presenting Complaint AVPU assessment Decides on placement Junior Doctor Secondary Assessment by Minors nurse, pick up card from box Presenting complaint Analgesia / ECG / Sometimes x-ray / sometimes Liaise PA Ambulance staff Pre-Reg Porter Places card in Box SpR / Consultant Porter Receptionist Resus Cubicle nurse X-ray Ambulance staff Porter Medical Assessment Nurse in Charge Secondary Assessment by nurse Radiographer Physician s Update Jonah with x-ray request Resus nurse Presenting complaint /VS Assistant Paper back-up PAT Nurse Junior Doctor Treatments Analgesia / ECG / Sometimes x-ray Liaise PA Co-ordinate transfers to ward and radiology Bloods/ Urinary Catheter SpR / Consultant Request bed on phone and Jonah Patient arrives at the Initial Assessment Porter Secondary Assessment by Doctor Arrive at an Inpatient bed Co-ordinate treatments ED by ambulance / police by PAT nurse Infection Control Presenting Complaint AVPU assessment Decides on placement Nurse in Charge Ops centre person Telephone handovers Check Treatments Ambulance staff Assessment 1 Cubicle nurse Check Coding Check VTE assessment SpR / Consultant Cubicle nurse Check swabs Patient registered by receptionist at bedside who returns to reception and then brings out front sheet back to nursing staff Secondary Assessment by nurse Treatments Presenting complaint /VS Medical Assessment Analgesia / ECG / Sometimes x-ray Liaise PA HCA / Cubicle nurse Ops centre person Porter CT Places Card in Box Junior Doctor Receptionist Radiographer Physician s Ambulance staff Nurse Coordinator Assistant Update Jonah with x-ray request CDU Paper back-up Bloods/ Urinary Catheter Co-ordinate transfers to ward and radiology SpR / Consultant Cubicle nurse Request bed on phone Treatments Ambulance staff Co-ordinate treatments Medical Assessment Telephone handovers Manage relatives Junior Doctor Request specialty Doctors to review Porter Ultrasound Assessment 2 Cubicle nurse Radiographer Cubicle nurse Secondary Assessment by nurse Treatments Physician s Presenting complaint /VS Assistant Analgesia / ECG / Sometimes x-ray Liaise PA Nurse Coordinator Places Card in Box Bloods/ Urinary Catheter SpR / Consultant Update Jonah with x-ray request HCA Paper back-up Nurse in Charge Ops centre person Co-ordinate transfers to ward and radiology Medical Assessment Cubicle nurse Treatments Request bed on phone Junior Doctor Co-ordinate treatments Telephone handovers Manage relatives Blue Chairs SAT Nurse PA cubicle Request specialty Doctors to review Secondary Assessment by SAT nurse Physician s Assistant Presenting complaint Analgesia / ECG / Sometimes x-ray Liaise PA Bloods Time Places Card in Box
Example: Rapid Cycle Methodology Analgesia for hip fracture patients Consistently identified as delayed RCEM Audit standard Identify a few failed standards that matter Repeat weekly on a small number of cases Feedback to whole staff, talk to staff about constraints Repeat as necessary
Workshop Design a rapid cycle audit project Focus on a few / single standards or problems Measurement? Think pragmatically about how this would work Think what problems you might find How you d offer solutions
Close New ways of improving care Collective Continuous responsibility