Understanding Paroxysmal Nocturnal Hemoglobinuria (PNH) and G6PD Deficiency Anemias
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare acquired disorder causing hemolytic anemia due to red cell membrane defects, leading to increased sensitivity to complement. On the other hand, G6PD Deficiency is a genetic condition causing hemolytic anemia due to impaired function of the G6PD enzyme, rendering red cells vulnerable to oxidative injury. Clinical features, diagnostic tests, and associated risks of both conditions are outlined in detail by Dr. B.V. Vydehi, a Professor of Pathology.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
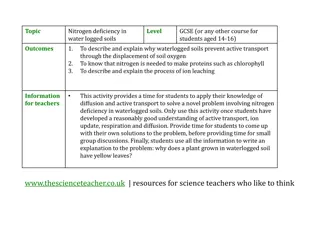
PNH AND G6PD DEFICIENCY ANEMIAS Dr. B.V.Vydehi M.D PROFESSOR OF PATHOLOGY NARAYANA MEDICAL COLLEGE,NELLORE
Paroxysmal Nocturnal Hemoglobinuria (PNH) Only hemolytic anemia caused by acquired defect in red cell membrane Rare disorder with undue sensitivity of RBC to complement due to defective synthesis of red cell membrane proteins 3 GPI Linked Proteins that regulate complement activity are deficient in PNH CD 55 (Decay accelerating factor), CD 59 (Membrane inhibitor of reactive lysis) & CD 8 binding protein
Paroxysmal Nocturnal Hemoglobinuria Mutation of Stem Cells - No Anchor Protein (Chronic Hemolysis) Acquired mutations in phosphatidyl inositol glycan A (PIGA) which is essential for synthesis of GPI anchor (Glycosyl phosphatidyl Inositol) C Complement- Induced Lysis (Intravascular) - Hb in Urine) C C
P N H - CLINICAL FEATURES Intravascular hemolysis is Paroxysmal & nocturnal in only 25 % cases Chronic episodic hemolysis without hemoglobinuria is more common Striking predisposition to intravascular thrombosis ; often involving hepatic, portal or cerebral veins accounts for 50% of deaths in PNH 20% of cases develop MPD or MDS or AML Specific tests : Ham s test & sucrose hemolysis test
G6-PD Deficiency-Hemolytic Anemia Deficiency or impaired function of G6 PD enzyme defective glutathione metabolism / HMP shunt abnormalities RBC vulnerable to oxidative injury hemolytic disease Red cells are vulnerable to injury by exogenous & endogenous oxidants
G6-PD Deficiency-Hemolytic Anemia Recessive X-linked trait : P/F to oxidant stress : - Drugs : Antimalarials, sulfonamides, Nitrofurantions, Aspirin, Vit.K Males at higher risk - Infections : Viral hepatitis, Pneumonia, Typhoid fever - Favism : Ingestion of fava beans
G6 G6- -PD deficiency PD deficiency- -Natural protection Natural protection from Malaria from Malaria Plasmodium cannot survive inside RBCbecause itneeds G6PD enzyme for its survival
G 6-PD Deficiency-Hemolytic Anemia Acute intravascular hemolysis : Anemia, hemoglobinemia & hemoglobinuria - Occurs 2 to 3 days following exposure of G6-PD deficient individuals to oxidants Supravital stain : Heinz bodies (Precipitates of denatured globins) Peripheral smear : Spherocytes & bite cells Bite cells are produced due to plucking of these inclusions by splenic macrophages
REFERENCES 1.Robbin & Cotran pathologic basis of diseases- 9th edition. 2.Harsh Mohan . Textbook of pathology -8th edition 3.Internet sources