Understanding the Process of Drowning and Its Implications
Drowning is a complex process that can have serious consequences on the body, leading to respiratory impairment and potentially fatal outcomes. This comprehensive overview delves into the definitions, classifications, and physiological aspects of drowning, shedding light on the various stages and contributing factors involved in the drowning process.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Drowning 7thApril, 2010 Amanda Diaz Intensive Care Unit John Hunter Hospital
Drowning in Oz Royal Lifesaving Society Australia (08-09) 302 drowning deaths 32 (11%) age 0 4 yrs 11 (4%) age 5 14 yrs 84 (28%) age 15 34 yrs 66 (22%) Males 80 (26%) age 35 54 yrs 94 (31%) age > 55 yrs 1.4 / 100,000 people (same as 1999 levels)
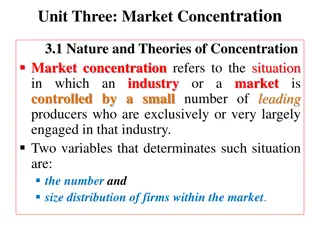
Definition of Drowning Confusing! Dictionary definition regards drowning as dying as a result of water filling the lungs preventing gas transfer and causing asphyxiation Sub-classifications based on dying (drowning) v not (near-); primary v secondary drowning (dying at the time or later); aspiration v non-aspiration
Definition of Drowning 2002 World Congress on Drowning (Amsterdam) Published in Circulation 2003: A process resulting in primary respiratory impairment from submersion/ immersion in a liquid medium. Liquid/ air interface present at the entrance of the victim s airway prevents them from breathing air. Survival is not considered in this definition
The Drowning Process: A Continuum Submersion Airway below surface Voluntary breath-holding Healthy volunteers 87s (longer with hyperventilation) Shorter (10-20 s) in water < 15 C Break-point results in involuntary ventilation Breath-hold can be prolonged with swallowing / active respiratory movement Laryngospasm when water stimulates epiglottis /oropharynx
The Drowning Process: A Continuum Respiratory movement against closed glottis Forced expiration against column of fluid: acute emphysema; alveolar septal rupture Decrease in alveolar / arterial pO2 Increase in alveolar / arterial pCO2 Hypoxaemia, acidosis, hypercarbia Critical hypoxia release of laryngospasm Aspiration
The Drowning Process: A Continuum Aspiration amount varies widely Up to 10% at autopsy have no evidence of aspiration Average 7 ml/kg aspirated 22ml/kg considered fatal aspiration Electrolyte disturbance from increase blood volume Up to 70% of drownings aspirate foreign material Algae Mud Vomitus
Why is drowning so complicated? Primary respiratory insult relatively easy to treat Major therapeutic challenge is the limitation of brain injury Identifying those with poor prognosis is extremely difficult No 2 drownings are alike
Factors Affecting Survival from Drowning Patient Factors: Age Co-morbidities / Intoxication Aspiration Core Body Temp Blood pH / Stress level during submersion Environmental Factors: Water Temperature Rescue Factors: Duration of submersion Time to effective BLS Time to return of spontaneous circulation No single clinical or lab value predicts morbidity or mortality
Age Older people tend to have more co-morbidities Decreased physiological reserve Children have a high body surface area : mass ratio Cool down faster Diving Response Ophthalmic division CN5 Marked generalised vasoconstriction, apnoea, bradycardia Hypometabolism Case Reports of children surviving submersion of up to 25 min (Nordic countries)
Aspiration 20% of drownings have normal CXR on admission At risk of ALI progression Water aspiration: As little as 2.2 ml/kg impairs O2transfer Freshwater aspiration: Affects surfactant phosphlipids leading to unstable alveoli, collapse, atelectasis Increases absolute shunt Hypotonic fluids directly cytotoxic Interstitial & alveolar oedema Saltwater (hypertonic): Direct acute alveolar oedema
Aspiration Bronchospasm Increases relative shunt Overall effect: Increase V/Q mismatch Decreased lung compliance Increased work of breathing
Hypoxia Lowers set-point to thermoneutral zone (normally 22-28 C) Worsens hypothermia in pre- & post-resuscitation phase Severe acid-base disturbance Increase anaerobic metabolism Increased catecholamine release Myocardial arrhythmias Coagulopathy DIC (endothelial cell activation)
Core Body Temperature Hypothermia: core temp < 35 C Rate of change of core body temp dependent on: Physical factors: water temp, movement of water against skin, insulation, head protection (increased heat loss via evaporation / convection / conduction) Physiological factors: BSA:Mass ratio, metabolic rate (affected by alcohol), peripheral circulation Cooling the fully clothed adult to < 35 C 1 hour in water at 5 C 2 hours in water at 10 C 3-6 hours in water at 15 C
Hypothermia: Cerebral Blood Flow Consciousness lost at 30 C Neurological protection only occurs if cerebral hypothermia induced before hypoxic damage occurs Studies done in anaesthetised humans Cerebral blood flow decreases in proportion to O2 requirements (autoregulation) 6-7% reduction in CMRO2 for each 1 C decrease in core body temp Cerebral activity abolished at < 22 C
BUT... If ventilating: Shivering at < 34 C Increased O2requirements Increased CO2/ lactate production If hypoxic: Set-point of thermoneutral zone lowered Shivering impaired Vasodilation of peripheries If hypercarbic: Cerebral vasodilation
Hypothermia: CV Function Arrhythmias occur any are possible Core temp < 28 C VF Core temp 24-26 C Asystole Why? At < 30 C Purkinje fibres lose conduction advantage over other ventricular muscle fibres
Hypothermia: Muscle Function Muscle (not core) temp < 28 C Impaired NMJ function Weakness Unable to swim
Hypothermia: Blood Increased blood viscosity Impaired coagulation Enzyme system
Youre Not Dead til Youre Warm & Dead Hypothermia has profound effects A & B if you re thinking the above ETT C: Fluid resuscitation in water, hydrostatic pressure increases vascular volume baroreceptor activation natiuresis & diuresis 2-3 L deficit on entering ED
Youre Not Dead til Youre Warm & Dead C: CPR - <28 C core body temp Manual compression CPR must be continued until core temp > 33 C Case reports of 4.5hrs manual compression CPR with successful neurological outcome Case reports of 6hrs with Thumper device Try defibrillation If not immediately successful, do not retry til > 29 C If successful, bear in mind reversion to VF is common until > 30 C
Youre Not Dead Til Youre Warm & Dead Warming: If core temp > 28 C, aim for 1 C/hr re- warming Active Re-warming (1-2 C/hr) Forced-air warming device (Bair hugger) Warmed fluid Warmed humidified gases Aggressive Re-warming (temp < 28 C) Bladder irrigation Gastric/pleural lavage Peritoneal Dialysis Haemofiltration
Re-warming Cardio-pulmonary bypass Fem-fem (partial) most common Shown to be beneficial with core temp < 25 C, regardless of rhythm Core temp 25-28 C is no benefit of CPB v conventional re-warming Can perform aorto-caval CPB Increases core body temp by 10 C/hr
When to stop Resuscitation considered futile when If core body temp 35 C Stable cardiovascular function cannot be achieved
Neurological Outcome Of those who arrive comatose survived intact survived with minor neurological deficit died or survived in a persistent vegetative state The only predictor proposed is regarding avalanche: K > 10 mmol/l indicates asphyxial cardiac arrest Not compatible with successful resuscitation
Cerebral Resuscitation Many modes tried Cooling / ICP monitoring / CPP targets None have been shown to produce improved morbidity or mortality Horse has already bolted
References 2009. Royal Life Saving Society Australia. The National Drowning Report 2009. http://www.royallifesaving.com.au//resources/d ocuments/2009_RLSSA_National_Drowning_Rep ort_Web.pdf Layon, J et al. Drowning: Update 2009. Anesthesiol. 2009; 110:1390. Hasibeder, WR. Drowning. Curr Op Anaesthesiol. 2003; 16:139 Golden, F St C et al. Immersion, near-drowning & drowning. BJA. 1997; 79:214