Understanding Eating Disorders: Overview, Prevalence, and Types
This detailed information covers the prevalence of eating disorders in the U.S., including statistics on anorexia, bulimia, and binge eating disorder. It also delves into the impact of eating disorders on children and adolescents, highlighting disturbing trends in body image and obesity rates. Additionally, the document explores various types of eating disorders such as anorexia nervosa, bulimia nervosa, binge eating disorder, and specifies diagnostic criteria and severity levels for anorexia nervosa.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
+ Overview of Eating Disorders Seda Ebrahimi Ph.D. Founder and Director of the Cambridge Eating Disorder Center Instructor, Department of Psychiatry, Harvard University
+THE PREVALENCE OF EATING DISORDERS An estimated 8 million Americans suffer from eating disorders 7 Million Women 1 Million Men 1 in 200 women in America suffer from anorexia 2-3% of American women suffer from bulimia Nearly 50% of all Americans know someone suffering from an Eating Disorder 10-15% of those suffering from anorexia or bulimia are males
+CHILDREN AND EATING DISORDERS 42% of third grade girls wish to be thinner 50% of 11-13 girls view themselves as overweight Obesity rates have tripled in children ages 2- 19 since the 1980s 32% are overweight 17% are obese Caucasian:10% boys, 15% girls African American: 17% boys, 23% girls Hispanic: 24% boys, 17% girls
+ DIFFERENT TYPES OF EATING DISORDERS Anorexia Nervosa Restricting type Binging/Purging Type Bulimia Nervosa Binge Eating disorder Other Specified Feeding or Eating Disorder Unspecified Feeding or Eating Disorder
+ANOREXIA NERVOSA Persistent restriction of energy intake leading to significantly low body weight (in context of what is minimally expected for age, sex, developmental trajectory, and physical health) . Either an intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain (even though significantly low weight). Disturbance in the way one's body weight or shape is experienced, undue influence of body shape and weight on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight. Subtypes: Restricting type Binge-eating/purging type
+ANOREXIA NERVOSA (CONTINUED) Specify if: In partial remission: After full criteria of anorexia nervosa were previously met, Criterion A (low body weight) has not been met for a sustained period, but either Criterion B or Criterion C is still met. In full remission: After full criteria of anorexia nervosa were previously met,none of the criteria have been met for a sustained period of time. Specify current severity: The minimum level of severity is based, for adults, on current body mass index (BMI) (see below) or, for children and adolescents, on BMI percentile. The ranges below are derived from World Health Organization categoriesfor thinness in adults; for children and adolescents, corresponding BMI percentiles should be used. The level of severity may be increased toreflect clinical symptoms, the degree of functional disability, and the need for supervision. Mild: BMI > 17 kg/m2 Moderate: BMI 16-16.99 kg/m2 Severe: BMI 15-15.99 kg/m2 Extreme: BMI < 15 kg/m2
+ANOREXIA NERVOSA WARNING SIGNS Low Weight Avoidance of Food Food rituals Excessive/compulsive exercise Body checking Body distortion and dissatisfaction Calorie counting Obsessional weighing If binging eating/purging: Laxative or diuretic ues Diet pills Binge eating Self induced vomitting
+BULIMIA NERVOSA Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: Eating, in a discrete period of time (e.g. within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances. A sense of lack of control over eating during the episode (e.g. a feeling that one cannot stop eating or control what or how much one is eating). Recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise. The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for three months. Self-evaluation is unduly influenced by body shape and weight. The disturbance does not occur exclusively during episodes of Anorexia Nervosa.
+BULIMIA NERVOSA WARNING SIGNS Cognitive distortions and irrational beliefs around, weight and appearance Body image distortions Body loathing May have food rituals Hiding or sneaking food Discomfort/avoidance of eating in public Obsessive weighing Body checking Frequent/Compulsive exercise Dieting/calorie counting
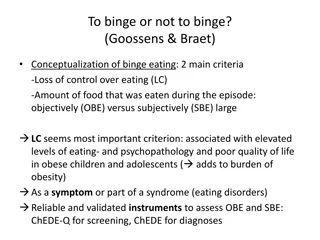
+BINGE EATING DISORDER (BED) Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following: Eating, in a discrete period of time (e.g. within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances. A sense of lack of control over eating during the episode (e.g. a feeling that one cannot stop eating or control what or how much one is eating). The binge eating episodes are associated with three or more of the following: eating much more rapidly than normal eating until feeling uncomfortably full eating large amounts of food when not feeling physically hungry eating alone because of feeling embarrassed by how much one is eating feeling disgusted with oneself, depressed or very guilty afterward Marked distress regarding binge eating is present Binge eating occurs, on average, at least once a week for three months Binge eating not associated with the recurrent use of inappropriate compensatory behaviours as in Bulimia Nervosa and does not occur exclusively during the course of Bulimia Nervosa, or Anorexia Nervosa methods to compensate for overeating, such as self-induced vomiting.
+Other Specified Feeding or Eating Disorder (OSFED) A diagnosis might then be allocated that specifies a specific reason why the presentation does not meet the specifics of another disorder (e.g. Bulimia Nervosa- low frequency). The following are further examples for OSFED: Atypical Anorexia Nervosa: All criteria are met, except despite significant weight loss, the individual s weight is within or above the normal range. Binge Eating Disorder (of low frequency and/or limited duration):All of the criteria for BED are met, except at a lower frequency and/or for less than three months. Bulimia Nervosa (of low frequency and/or limited duration): All of the criteria for Bulimia Nervosa are met, except that the binge eating and inappropriate compensatory behavior occurs at a lower frequency and/or for less than three months. Purging Disorder: Recurrent purging behavior to influence weight or shape in the absence of binge eating Night Eating Syndrome: Recurrent episodes of night eating. Eating after awakening from sleep, or by excessive food consumption after the evening meal. The behavior is not better explained by environmental influences or social norms. The behavior causes significant distress/impairment. The behavior is not better explained by another mental health disorder (e.g. BED).
+COMMON EATING DISORDER WARNING SIGNS Preoccupations with body or weight Obsession with calories, food or nutrition Constant dieting even when thin Rapid unexplained weight loss or weight gain Taking laxatives or diet pills Compulsive exercising Making excuses to get out of eating
+ COMMON EATING DISORDER WARNING SIGNS (CONTINUED) Avoiding social situations involving food Going to the bathroom right after meals Eating alone, at night or in secret Hoarding high-calorie food Fainting Wearing many layers of clothing Redness on backs of hands Chipmunk cheeks Dental problems
+RECURRING WARNING SIGNS Excessive talk of exercise Lots of food/diet talk Fat Talk Negative body image Low self-esteem Self-deprecating Complaints of constipation (laxative use) Amenorrhea/menstrual irregularity
+MEDICAL COMPLICATIONS Fatigue Anemia Weakness Brady Cardia Sleep disturbances Hypotension Dizziness/fainting Hypothermia Chest pain Chest pain Osteoporosis/Osteoperia Edema Amenorrhea Amenorrhea Cold Intolerance Swollen Parotid Glands Brittle hair/nails Dental Erosions Abdominal pain Knuckle scarring Constipation/diarrhea Electrolyte imbalance Hair loss Sore Throat
+Common Comorbidities Depression Generalized Anxiety Social Anxiety OCD Alcohol/substance abuse Borderline Personality Disorder Trauma History Self-harming behaviors
+Multidisciplinary Treatment Team Approach Medical Stability Medication Management Nutritional Rehabilitation Psychotherapy
+Eating Disorders and Nutrition Normalization of eating Weight Restoration Re-feeding Issues Activity Level
+Goals of Treatment Restoration of weight Normalization of eating Significant changes in thoughts and behaviors Relapse prevention
+Behavioral warning signs Focus on low-fat or heathy foods Diet drinks Energy bars Supplements Counting calories and grams of fat Becoming vegetarian/vegan Fasting Obsessive thinking about food Skipping meals/refusal to eat Avoiding food in social situations Wearing oversized clothing Complaining of food allergies Excessive exercise Reading fitness/health magazines Checking weight several times daily Body checking Spending excessive amounts of time in front of the mirror
+Psychological Signs of at-risk Individuals Perfectionism Competitiveness Overly responsible Critical of self/others Conformity Approval seeking Low self-esteem Mood swings Rigid black and white thinking Difficulty expressing emotions Complaining of feeling fat
+SOCIAL SIGNS OF AN AT RISK INDIVIDUAL Isolation Avoidance of social/recreational activies Dieting schedule Exercise regimen
+HOW TO ADDRESS AN AT-RISK INDIVIDUAL Early intervention is crucial to recovery Show support and concern Express empathy and understanding Be truthful in addressing denial and resistance Be aware of local resources and make appropriate referrals for assessment and treatment
+TREATMENT Creating the Treatment Team Building the Treatment Contract Psycho-education Building trust and rapport Different Therapeutic Methods Cognitive Behavioral Therapy (CBT) Dialectical Behavior Therapy (DBT) Family-Based Treatment (FBT/Maudsley Method) Psychodynamic Therapy
+TREATMENT LEVELS OF CARE Outpatient Intensive Outpatient Partial Hospitalization (Day Treatment) Transitional Living Residential Inpatient (Acute Hospitalization)
+CRITERIA FOR INPATIENT TREATMENT Low weight (severity, rapidity) Alterations in vital signs (postural hypotension, Bradycardia) Low Serum Potassium level (fatal arrhythmia) Low Mood (Suicidal thoughts or intents) Presence of Formal Thought Disorder Presence and severity of associated Impulsivity Control Problems (e.g. sexual promiscuity, shoplifting, financial difficulties, alcohol/drug abuse, self injurious behaviors) Level of disruption to daily functions Job difficulties/loss of job Withdrawal from school Isolation Failure of outpatient treatment
+Treatment Contract Certain amount of weight loss leading to higher level of care Not gaining weight leading to a higher level of care Frequency of weight checks, blood work, etc. Activity level specifications Frequency of binge/purge may require a higher level of care One person is identified as the leader of the team; generally the individual therapist Splitting can be a major problem Frequent communication is a must
+TREATMENT AT CAMBRIDGE EATING DISORDER CENTER Specialized Multidisciplinary Eating Disorder Treatment Including: Individual therapy Family therapy Group therapy Nutritional Support/education CBT/DBT/FBT Medication management Expressive arts therapy Yoga Levels of Care include: Residential Partial Hospitalization Intensive Outpatient Outpatient Transitional Living Teaching Facility: Harvard University Psychiatry Massachusetts General Hospital
+Seda Ebrahimi Director, Cambridge Eating Disorder Center Cambridge Eating Disorder Center (CEDC) 3 Bow Street | Cambridge, MA 02138 617-547-2255 ext. 222 seda@cedcmail.com www.eatingdisordercenter.org
+ Questions?