Pediatric Respiratory Infections: An Overview of Cases and Physiology
This review delves into selected cases of respiratory infections in children presented by Dr. David L. Smith, focusing on the anatomical and physiological aspects of the pediatric airway and respiratory system. It discusses respiratory failure in infants and small children, metabolic demands, cyanosis, and the comparative anatomy of the pediatric and adult respiratory systems. The presentation illuminates key differences in pediatric respiratory physiology, emphasizing the importance of understanding these nuances in providing effective care for young patients.
- Pediatric Respiratory Infections
- Pediatric Airway
- Respiratory System
- Childrens Health
- Anatomical Differences
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
Respiratory Infections in Children A brief review of selected cases David L. Smith, MD, FAAP Pediatric Intensivist
new stuff has come to light, and some old stuff is worth repeating (the Dude circa 1998) OBJECTIVES: Review anatomic and physiologic aspects of the pediatric airway and respiratory system Discuss selected aspects of resp. care in infants/children Case presentations
Respiratory failure more common in infants/small children due to immaturity in 4 areas: CNS receptor and effector mechanisms for resp. drive Metabolic rate 2 to 3 times the O2 consumption / REE of adult Chest wall stability and muscle strength Conducting airways and the alveolar-capillary complex
Metabolic/physiologic Demand A child has 2-3 times the oxygen consumption rate of an adult! Resp. Distress/increased work of breathing in infants and small children can divert in 30-40% of cardiac output to muscles of respiration!
Cyanosis Poor indicator of hypoxemia in children Greater than 5 g/dl of total hemoglobin de-saturated before clinically evident Dependent total hemoglobin concentration - less in children, and certainly less in the face blood loss
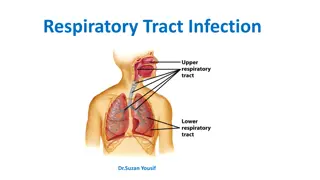
PEDIATRIC AIRWAY & RESPIRATORY PHYSIOLOGY S. Kache, MD The respiratory mechanism of the pediatric patient varies from the adult in both anatomy and physiology. As children grow, the airway enlarges and moves more caudally as the c-spine elongates. The pediatric airway overall has poorly developed cartilaginous integrity allowing for more laxity throughout the airway. Another important distinction is the narrowest point in the airway in adults is at the cords versus below the cords for children. Some of the important anatomic differences are listed below. The Pediatric Airway RESPIRATORY SYSTEM COMPARATIVE ANATOMY: Anatomy PEDIATRIC ADULT Tongue Large Normal Eiglottis Shape Floppy, omega shaped Firm, flatter Epiglottis Level Level of C3 - C4 Level of C5 - C6 Trachea Smaller, shorter Wider, longer Larynx Shape Funnel shaped Column Larynx Position Angles posteriorly away from glottis Straight up and down At level of Vocal cords Narrowest Point Sub-glottic region Lung Volume 250ml at birth 6000 ml as adult An important aspect of the narrow airway in children is that resistance is significantly increased. The formula to consider is R ~ 8l / r4 R resistance, l length, r radius Small changes in the airway radius will therefore increase the resistance to the fourth power. Therefore, a small amount of post-extubation sub-glottic edema will significantly increase the work of breathing for an infant. Children also have a smaller forced residual capacity (FRC) defined as the residual volume plus the expiratory reserve volume. Physiologically, FRC occurs when the outward pull of the chest wall equals the inward collapse of the lungs. Pediatric Airway & Respiratory physiology 1
AIRWAY RESISTANCE Hagen Poiseuille law: R = 8 l n / r4
Intra- vs extra-thoracic airway obstruction
Clinical features of respiratory distress
Clues to upper vs. lower airway noises Monophonic vs. Polyphonic Phase of respiration I:E ratio
Case # 1 4 m/o male 3 day h/o nasal congestion Temperature max of 101.5 degrees F Inspiratory stridor Decreased fluid intake Radiograph:
Diagnosis ? VIRAL CROUP
Why heliox? Reynolds number is the ratio of inertial forces to viscous forces within a fluid
Case # 2 4 y/o female Abrupt development of fever to 102 Will not speak Drooling unimmunnized
CROUP EPIGLOTTITIS COMMON RARE 3 months to 3 years 3 7 years URI Prodrome Abrupt onset Barky cough, stridor (non- toxic) Stridor(TOXIC) 3 D s and a T Fever < 39 C Fever > 39 C WBC Ct. normal WBC Ct. Elevated X-Ray = steeple sign X-ray = thumb sign
Initial Management of Epiglottitis Suspected Epiglottitis Child in Mom s Lap no interventions Notify OR,ENT, Anesthesiologist, intensivist IV Access, PICU, 3rd Gen. Cephalosporin Artificial(surgical) airway in OR
Case #3 7 y/o male Inspiratory stridor present acutely with fever to 101 F toxic appearance, stridor, tachypnea WBC count 35,000 Cough is not painful prodrome of an upper respiratory infection
Case #3 Child has a barky cough Stridor does not respond to racemic epi neb Sudden decompensation requiring intubation What s the diagnosis? Bacterial tracheitis
Etiologies of bacterial tracheitis S aureus: Community-associated methicillin-resistant S aureus (CA-MRSA) S pyogenes Streptococcus pneumoniae Moraxella catarrhalis: is a leading cause of bacterial tracheitis and associated with increased intubation. Haemophilus influenzae type B (Hib): This cause is less common since the introduction of the Hib vaccine.
Management of bacterial tracheitis maintenance of the airway fluid resuscitation (if needed) administration of appropriate antimicrobial agents Some children require emergent or urgent evaluation of the airway via endoscopy generally best performed in the operating room
Case #4 1 m/o presents to ER with 2 brief episodes of apnea No h/o nasal congestion or cough One episode if apnea lasted ~ 30 seconds and resulted in central cyanosis 3 y/o sister attends daycare has a viral URI Infant has been listless and not feeding well for ~ 12 hours
Your diagnosis please? Bronchiolitis
Is RSV induced apnea obstructive or central? CENTRAL Extrapulmonary manifistations of RSV include: cardiovascular failure - myocardial damage as evident from elevated cardiac troponin levels (35-54% of ventilated infants) cardiac arrhythmias (supraventricular / ventricular tachycardia) central apnea (16-21% of admissions) seizures / focal neurological abnormalities hyponatraemia (33%) - SIADH hepatitis (46-49% of ventilated infants) RSV or its genetic material have been isolated from cerebrospinal fluid, myocardium, liver and peripheral blood
Case #5 6 m/o male who was a term infant no perinatal complications Has been healthy up until the past few days vomiting No h/o fever WBC count 32,000 WBC differential: 15% segs, 2% bands, 80% lymphs, 3% eos Your diagnosis please! pertussis
Case #6 4 y/o female presents to clinic with fever to 103 F which began last night Now with N/V and severe abdominal pain Rapid strep negative Flu PCR negative Clean catch UA negative WHAT TEST DO YOU WANT NEXT?
Bacterial Pneumonia-Etiologies Typical: Pneumococcal Haemophilus Influenzae Moraxella Staphylococcal Atypical: Mycoplasma Legionella Chlamydia Q Fever Psittacosis
Case #7 2 w/o neonate born at 36 weeks EGA Uneventful nursery course No fever Purulent eye drainage CBC: WBC count is 14,500 Diff: 30% segs, 5% bands, 15% lymphs, and 50% eosinophils Your diagnosis please! chlamidia
WHAT ANTIBIOTIC IS APPROPRIATE FOR THE TREATMENT OF CHLAMIDIA? A MACROLIDE (ERYTHROMYCIN)
Recently discovered virus in the herpes family with a bird vector? CHIRPIES It s a cannarial disease It s untweetable Reference: New England Journal of Irreproducible results: 30:3, 2016
These little Squalls, they come on ya fast and they leave ya fast
Lecture evaluation Answers: Yes Did Dr. Smith s feeble attempts at humor detract from his message? What, in fact, was his message? Unclear, at best Yes Were the TV/movie references outdated? Whose counting Yes How many times was the word dude used in the presentation? I should hope so! Would you describe the talk given by Dr. Smith as stream of consciousness or word salad? Highly unlikely! Was the talk ecumenical? Will Dr. Smith be asked to speak at an upcoming respiratory symposium?