Combat Rising Healthcare Costs with Advanced Medical Pricing Solutions
Partnering with Advanced Medical Pricing Solutions (AMPS) helps combat rising healthcare costs by auditing facility claims, ensuring fair pricing, and disputing excessive charges. It's crucial to match EOB and billing amounts, contact BAS customer service immediately, and take steps to avoid balance billing. Patient responsibility is critical, and timely payments are necessary for protection against overbilling. Contact BAS at 1-800-843-3831 for assistance.
- Healthcare costs
- Advanced Medical Pricing Solutions
- Billing practices
- Patient responsibility
- Balance billing
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. Download presentation by click this link. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
E N D
Presentation Transcript
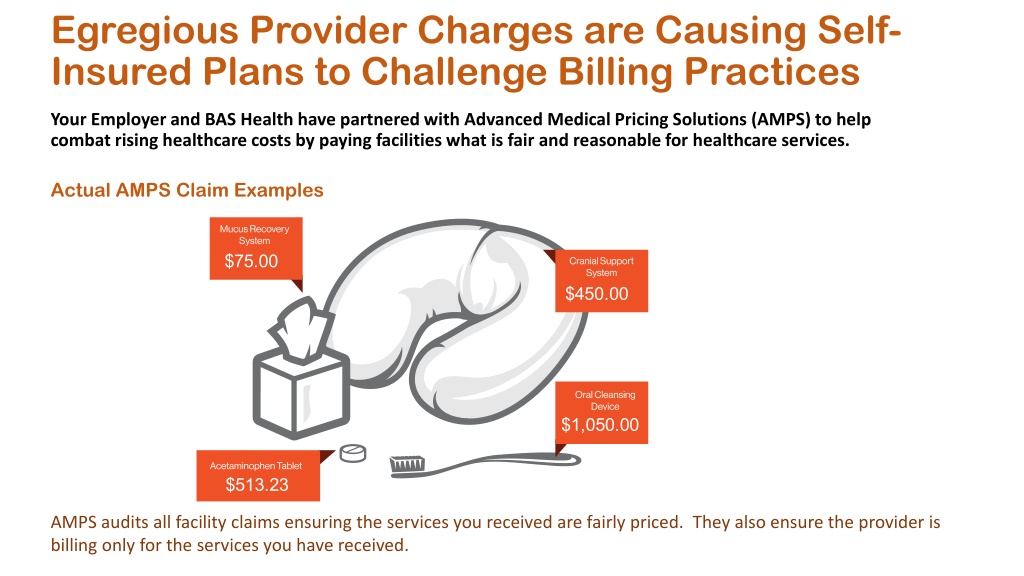
Egregious Provider Charges are Causing Self- Insured Plans to Challenge Billing Practices Your Employer and BAS Health have partnered with Advanced Medical Pricing Solutions (AMPS) to help combat rising healthcare costs by paying facilities what is fair and reasonable for healthcare services. Actual AMPS Claim Examples AMPS audits all facility claims ensuring the services you received are fairly priced. They also ensure the provider is billing only for the services you have received.
EOB and Bill Must Match! Provider bill shows the member owes $261.00. This does not match the EOB. Call BAS Immediately! EOB shows the member owes $150.00 The amount owed is different from the EOB. CALL BAS
Remember: Contact BAS Customer Service Immediately Your Responsibility: 1. Make sure the bill you receive matches your EOB. 2. Confirm you ve paid your patient responsibility indicated on your EOB. 3. If the bill indicates you owe more than the patient responsibility outlined on your BAS EOB, call us immediately! AMPS will work on your behalf by disputing the excessive charges with the provider. Do NOT pay additional money to the provider! You must let BAS know within 60 days of receiving your first billing statement Uncertain if you are being balance billed? Call BAS at 1-800-843-3831 and we will help you Once AMPS is notified of a balance bill or collections attempt, a Balance Bill Kit will be sent to you for signature. This allows AMPS Advocates to work directly with the Provider regarding the benefit plan, payment determination and optional appeal process. AMPS will keep you updated on communications with the Provider and answer any of your questions that may arise.
BAS Customer Service & AMPS Team up BAS is your first contact to determine if you are being balance billed We will work with you to determine if you are truly balance billed and that you don t owe. (You may owe your deductible, coinsurance or uncovered services.) If you are being balance billed, we will transfer you to AMPS so the balance bill appeal process can begin. Use the BAS on-line tools to assist you View your claim Ask a question Download paperwork Subrogation forms, other Insurance forms, claims form
AMPS Welcome Letter Patient Responsibility is Critical Patient Responsibility is Critical If you can t pay the patient responsibility in full as shown on your EOB, then make a good faith effort and pay what you can. Do not sign any agreement stating you ll pay more than the patient responsibility. Failure to make timely payments consistently will limit our ability to protect you against balance billing or entering into a payment plan for more than patient responsibility. Be Patient! Be Patient! The Plan wants to stand firm on why they want to pay paying a fair price for services. Many claim issues can be resolved in a few months, but some can take up to 18 months to resolve. BAS can be reached at 1-800-843-3831 and we will help you!
Controlling the Cost of Health Care Here s how the claims process works: After AMPS receives your claim, AMPS Member Advocates will contact you via a Welcome Letter and/or phone call. AMPS is there to assist you should you receive any additional request for payment from the Provider.
When to Contact AMPS DOCUMENTS NEEDED TO BEGIN ADVOCACY PROCESS Explanation of Benefits (EOB) Provider Bill Proof of Payment of Patient Responsibility Signed Balance Bill Kit Fair Credit Billing Act (FCBA) 60-days starts from the date on the first Provider Bill you receive Not the Date of Service! If the claim exceeds $1500 you should expect a courtesy call from our Patient Advocacy Team 15-days after the Welcome Letter has been mailed. To protect you, AMPS will contact the 3 major credit reporting companies to advise them you have a bill that is being challenged
Important to Remember Member Advocacy Team Check Your Mail Monday Friday 8 am to 7 pm EST (Multilingual Advocates Available) Remember: 60 Day Timeline